With the new Payment Risk feature within the Denials Predictor module in MDaudit, providers can understand RCM compliance and financial risks associated with their most profitable services and specific payers.
MDaudit is truly differentiated in providing continuous risk monitoring (CRM) capabilities across the healthcare revenue cycle management (RCM) continuum. It’s our long-held conviction that most denials in the back end of the revenue cycle are triggered by billing, coding, and clinical issues upstream. When anomalies and abnormal events in these areas are proactively and continuously monitored in the mid-revenue cycle and fixed, compliance and revenue outcomes don’t have to compete as conflicting interests. Instead, they can become more strategic and sustainable versus transactional and temporal. This is the simple rationale from which we began our quest of building a world-class risk monitoring platform a few years ago that can unlock billing, coding, and revenue risks from various data sources like Charges, Denials, Internal Audit Insights, Payer Behavior, and more. This is why billing, coding, and revenue teams in leading health systems work out of a single enterprise platform in MDaudit to drive enterprise outcomes.
MDaudit’s Denials Predictor
MDaudit’s data shows clinical documentation and medical necessity-related necessity initially denied by payers increased by 51% from 2021 – 2023. The OIG estimated recently that the Part B and enrollee spending on these biologics could have decreased by $179 million, or 4 percent if more affordable biosimilars had been used as frequently as the most used biosimilars. Hence the necessity to prescribe branded drugs vs. biosimilars is being scrutinized for clinical denials. MDaudit’s Denials Predictor module serves as a pre-payment charge review engine specifically designed to address denials associated with their most profitable services attributed to Information Needed, Documentation Needed, and Medical Necessity. Denials Predictor enhances existing claim scrubbers by focusing on Specialty Drugs, Implants, and complex diagnoses within various healthcare settings such as hospitals, outpatient facilities, ambulatory surgical centers (ASCs), and inpatient facilities.
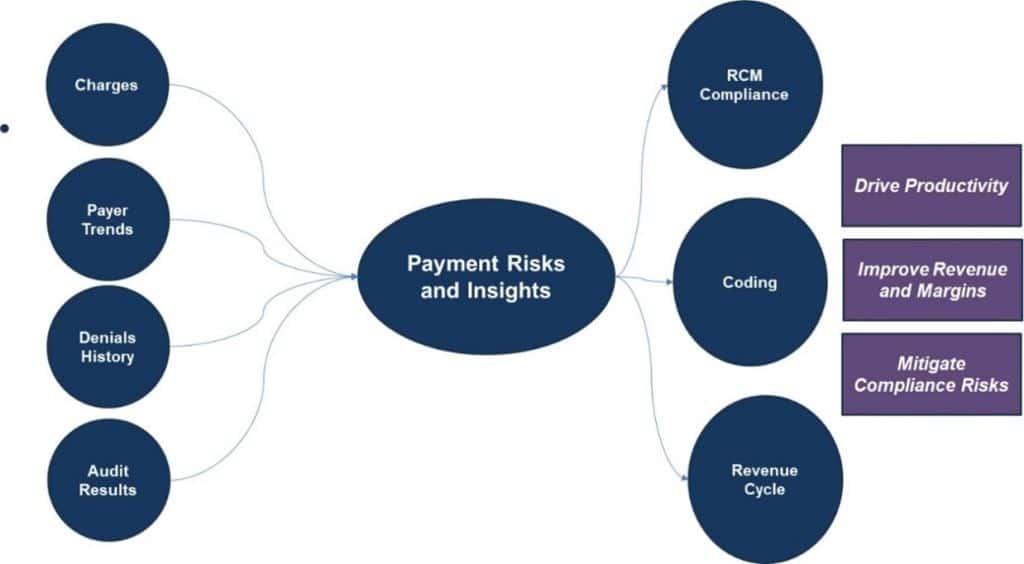
MDaudit’s Denial Predictor leverages multiple data sources to drive payment risk insights for various Provider Teams
New Denials Predictor Feature: Payment Risks
In response to customer feedback, we’re excited to introduce a new feature within Denials Predictor called Payment Risks. Payment Risks showcases summaries of historical denial data based on top denied codes and payer combinations along with individual accounts that have been flagged with these codes and payers allowing you to drive actionable outcomes through the integration with the auditing workflow.
With MDaudit’s NEW Denials Predictor Payment Risks, customers can now:
- Review up to six months of historical flagged claims, categorized by Rule Categories and flagged amounts.
- Reveal top denial trends and recommended corrective actions to mitigate recurrence
- Perform audits on the flagged claims and resolve issues systematically by educating providers, coders, and clinicians.
- Drill down by the top five providers, coders, payers, and facilities representing the whole or individual rule or rule groups.
- Creates a holistic view of denial workflows.
- Work in collaboration as an organization to manage denials, reduce risk, and enhance revenue.



