Revenue performance is under pressure in healthcare organizations across the country. These systems are juggling rising operating costs, staffing shortages, and growing scrutiny from payers and regulators. At the same time, their leaders are fighting an uphill battle to protect revenue, support clinical teams, and keep access to care strong.
A 2025 benchmark report supplies data supporting these trends:
- Risk-based audits increased 25% this year as more compliance teams lean on real-time data to surface risks earlier.
- HCC-based audits increased 102% this year.
- 30% rise in prospective or pre-bill audits
The revenue cycle has become too complex to manage with isolated tools and manual processes. The industry needs connected insights, fewer blind spots, and a way to stay ahead of billing risks before they become denials or takebacks.
This is why MDaudit exists. Our platform provides organizations with a connected view across the front, middle, and back end of the revenue cycle. The goal is simple: to help teams reduce preventable risk, maintain clean revenue, and make every audit effort count. We are your bridge to revenue integrity assurance.
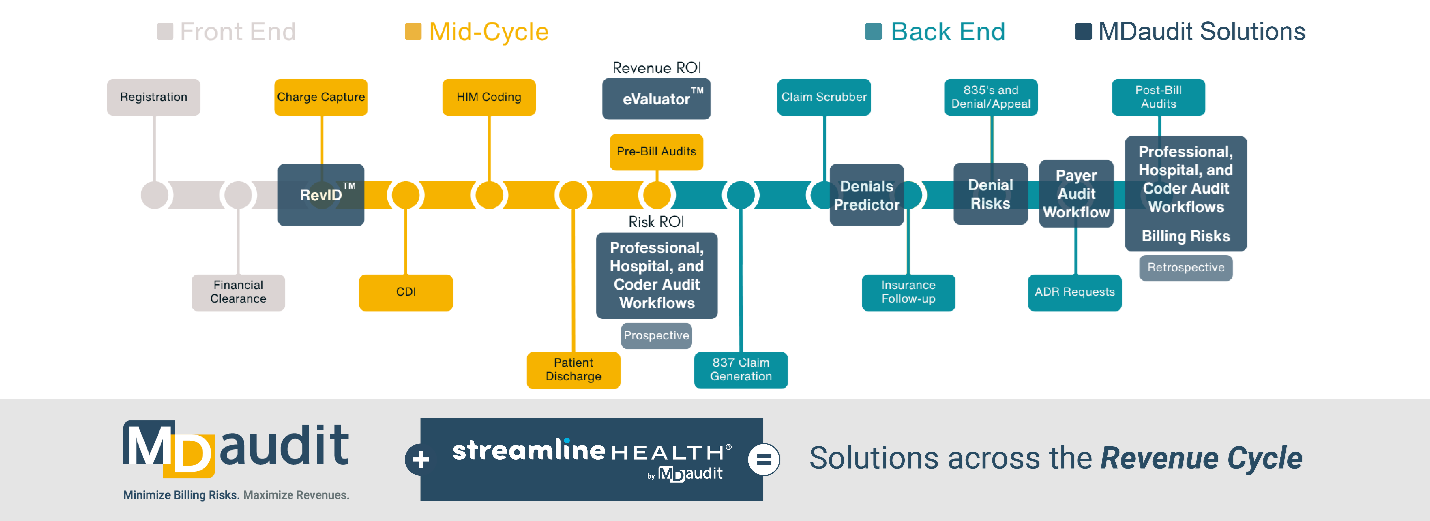
A Connected Approach to Revenue Integrity
As the infographic above illustrates, each stage of the revenue cycle carries its own exposure points and opportunities, and many teams along the cycle still operate in silos. Coding reviews sit apart from denial management. Charge capture and documentation accuracy operate on different timelines. Payer audits come late, leaving limited room to respond.
By integrating continuous monitoring, audit workflows, and predictive insights, teams get a shared view of where revenue is at risk and what actions can protect it. MDaudit delivers connected revenue integrity solutions that bring together front, mid, and back-end oversight.
Strengthening Mid-Cycle Accuracy
Mid-cycle is often where revenue exposure begins. Coding and Health Information Management (HIM) leaders know how easy it is for coding errors, documentation gaps, or charge capture issues to cascade into denials later.
MDaudit supports this stage of the revenue cycle with solutions that help teams identify issues early, provide targeted education, and maintain coding accuracy at scale. Bringing this layer of insight into daily operations helps organizations protect revenue before claims ever reach a payer.
Supporting Back-End Outcomes with Greater Predictability
Denials remain one of the costliest obstacles for healthcare systems. Payers continue to introduce new requirements and accelerate audits, leaving teams working reactively.
MDaudit’s denial prediction capabilities give leaders clarity on where denials are likely to occur and why. Combined with automated workflows for payer audits and appeals, teams spend less time gathering data and more time solving root-cause problems. This supports cleaner claims, faster reimbursement, and more stable financial performance.
Closing the Loop with a Unified Risk View
Executives need a reliable way to understand where exposure exists today and how it may change tomorrow. MDaudit provides that view through continuous risk monitoring across coding, billing, and reimbursement activities.
This unified approach helps organizations:
- Reduce preventable denials
- Strengthen compliance
- Improve audit accuracy and value
- Increase visibility into payer behavior
- Maintain greater control over revenue performance
When each part of the revenue cycle works from the same foundation, teams can focus on supporting clinicians, improving documentation, and building a stronger financial future.
Revenue Integrity Solutions that Deliver
Now that we’ve established what connected revenue integrity assurance looks like, let’s explore the solutions that healthcare organizations are using to minimize risks and maximize revenue.
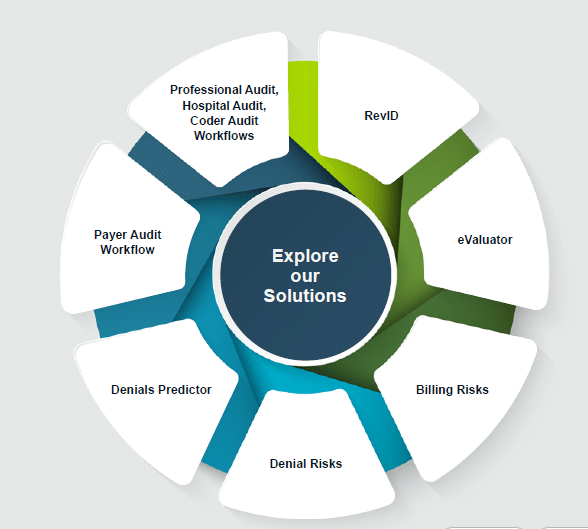
eValuator
eValuator is a pre-bill, coding integrity, and net revenue generating solution that provides 100% automated analysis of pre-bill charges to ensure they are both coded accurately and at the same time recognize the maximum amount of reimbursement. This will equate to fewer days in A/R, significantly lower denial rates, and, of course, healthier bottom lines.
RevID
RevID prevents missed and late charges with a cloud-based solution that enables automated compilation and analysis of all charge data to identify discrepancies between clinical activity and billing data for daily reconciliation.
Billing Risks
Billing Risks leverages the charge data ingested regularly from your organization’s claims to bring new insights to healthcare billing compliance and revenue integrity teams. The drill-down dashboards and reports allow you to detect billing and coding anomalies and determine root cause, or risk, with pre-built analytics and peer benchmarking tools. Easily identify opportunities to improve revenue and establish risk-based auditing practices.
Denial Risks
Denial Risks is a rich data analysis toolset powered by Augmented Intelligence (AI) to bring speed to insights and transparency on root cause of denials. Harness the power of analytics to help your organization mitigate avoidable denials and maximize revenue opportunities.
Denials Predictor
Addressing the charges that drive 80% of denial dollars that traditional claim scrubbers miss, Denials Predictor helps healthcare organizations get paid on initial claim submissions, avoiding costly appeals and write-offs, while empowering revenue integrity professionals to proactively identify and resolve claims likely to result in denials or delays prior to payer adjudication.
Payer Audit Workflow
Managing third-party governmental and private payer audits, such as Recovery Audit Contractors (RAC), Targeted Probe and Educate (TPE), and Comprehensive Error Rate Testing (CERT) audits, can be challenging without the right tools. The manual effort of tracking requests, pulling records, reporting results, and staying on top of due dates is time-consuming and inefficient. Payer Audit Workflow makes it easy to manage external audit requests on a single centralized, secure platform.
Audit Workflows
Audit Workflows offer a comprehensive solution for reviewing all chart types within your organization, including hospital, professional, and coder records, both prospectively and retrospectively. Audits can be more efficiently managed through templated and customizable workflows, automated schedules, task assignments, and digital document management. Additionally, providing robust audit reporting capabilities with advanced analytics dashboards enables users to quickly uncover valuable insights.
The Path Forward for Health Systems
Healthcare leaders cannot afford fragmented oversight. The revenue cycle is evolving quickly, and organizations need a partner that provides clarity, automation, and actionable insight.
At MDaudit, our focus is on helping you optimize revenue, supporting your teams, and operating with confidence. A connected, risk-aware, and data-driven revenue cycle is within reach, and we’re committed to helping organizations get there. Request a demo and discover revenue integrity solutions tailored to your specific needs wherever they may fall along the revenue cycle.