THE CUSTOMER PROFILE
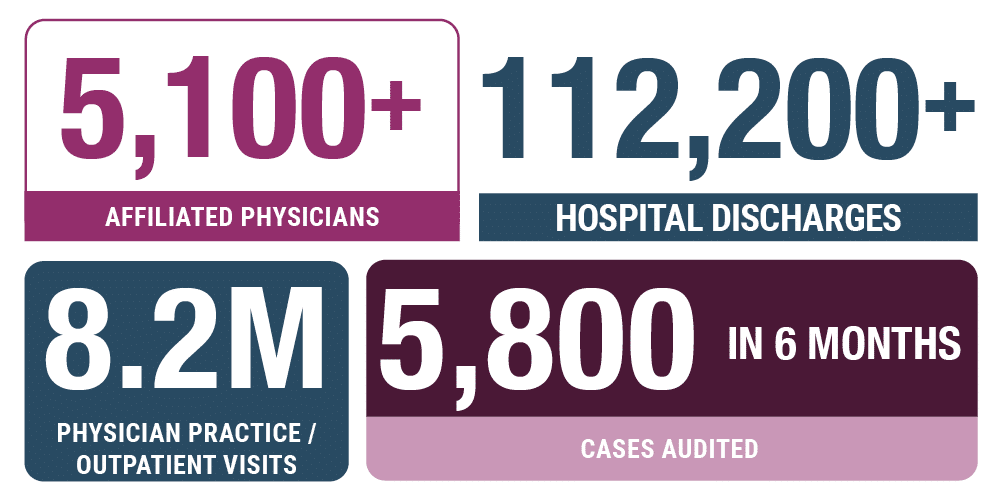
Prisma Health is the largest healthcare organization in South Carolina, with nearly 2,500 beds across 18 acute and specialty care hospitals and 300 outpatient sites. The nationally recognized private nonprofit health company employs 29,500 team members across its clinically integrated inVio Health Network.
Along with inVio, Prisma Health serves almost 1.5 million patients annually in its 21-county market area that covers 50% of South Carolina. Additionally, nearly 7,700 healthcare students attend medical residencies, internships, and other training programs each year through partnerships with over 140 affiliated medical, nursing, pharmacy, and allied health schools. These include the University of South Carolina, Clemson, and Furman.
THE CHALLENGE
A paper-based ambulatory compliance department required advanced technology for more efficient, effective auditing and expanded reporting.
In the wake of the merger between Palmetto Health and the Greenville Health System that created Prisma Health, the ambulatory billing compliance department found itself in the position of managing double the workload with less staff and manual processes. Its reliance on spreadsheets limited the scope of provider audits and made proactive identification of trends and potential problem areas impossible.
“You can’t necessarily see some things when you’re using manual audit processes,” said Tara Farmer, Ambulatory Compliance Officer, Prisma Health. Complicating matters were variances in the types and capabilities of the spreadsheet software used across regions. “The processes were just a little bit different in each region. Some compliance departments were able to take steps to automate certain functions by building formulas and creating dashboards in their spreadsheet software, which allowed running totals to be maintained. Elsewhere, the processes were more manual.”
Limited to dashboards for only the most labor-intensive information aggregation processes, the department could pull only a small number of reports and only quarterly – and only after a painstaking process of manual data entry. Further, the department had limited access to critical data around claims processing and denials. “To make decisions around risk, we had to work with what had been identified in the past or rely on things like word of mouth” about where issues might exist, said Farmer.
It quickly became clear that post-merger, even partially manual processes were untenable. “As a large healthcare system, we knew we were going to have more eyes on our processes; we needed to do something to protect the organization,” said Farmer. “We knew we needed to fully automate.”
At a previous healthcare organization, Farmer had participated in a demonstration of an early iteration of MDaudit and knew that MDaudit “would take us into the current century.”
As a large healthcare system, we knew we were going to have more eyes on our processes; we needed to do something to protect the organization. We knew we needed to fully automate.
We’ve been able to take the information obtained from MDaudit back to clinical leaders within Prisma that show specifically where change is needed. As a result, we’re starting to really see improvements and we’re creating conversations about what may have been missed in the past.
THE SOLUTION
MDaudit delivers advanced functionality and automation to enable the implementation of a risk-based auditing strategy.
Powered by sophisticated analytics and augmented intelligence, MDaudit enables healthcare organizations to reduce compliance risk, improve efficiency, and retain more revenue streams by providing workflow automation, risk monitoring, and built-in analytics and benchmarking capabilities in a single integrated cloud-based platform. By combining automated workflows with continuous risk monitoring and anomaly detection, the platform lets organizations quickly identify risks, determine the root cause of errors, and apply corrective actions to prevent future losses.
Further, MDaudit’s audit workflows provide the tools healthcare organizations like Prisma Health need to automate time-consuming tasks for a more strategic, risk-based approach to auditing. Since implementing MDaudit, Farmer and her team can continuously monitor key risk metrics and make data-based decisions on which providers should be audited – a far more efficient and effective strategy than basing audit decisions on how long it had been since a provider had been reviewed.
MDaudit also enables the compliance team to set up custom metrics. For example, to ensure compliance with new regulations around split/shared E&M (evaluation and management) services, the team created two new admission metrics, one for critical care and one for hospital rounds. “The changes with split/shared services are significant. With this year being somewhat of a grace period, we have time to work on this area. MDaudit gives us the ability to see where we need to audit. It gives us the ability to identify departments and quickly pull an audit on that area to see what we’re missing based on the regulatory changes,” said Farmer.
With MDaudit, the Prisma Health ambulatory compliance team targets education to shore up areas of weakness, such as the use of CPT Code 99211 for E&M at an office or outpatient visit with an established patient. Once audits identified this as a problematic code, Farmer’s team worked closely with coding education to get information into the hands of providers to facilitate the behavioral changes necessary to bring documentation and coding into compliance.
“We’ve been able to take the information obtained from MDaudit back to clinical leaders within Prisma that show specifically where change is needed,” said Farmer. “As a result, we’re starting to really see improvements and we’re creating conversations about what may have been missed in the past.”
Farmer counts reporting and the ability to communicate across the health system as one of the most valuable benefits of MDaudit. Sharing targeted data with leadership in real-time during Prisma’s bi-annual meetings with department chairs, meetings with medical group executive leaders, and with the health system’s chief financial officer is something that could not have been done using the former manual, spreadsheet-based system. With MDaudit, Farmer can delve into audit insights and tailor them to her audience for optimal impact, for example presenting data to the CFO on the medical group as a whole and department-over-department for chairs.
“We’re able to give an executive summary of what we’re seeing in MDaudit, areas that should be more closely monitored for the organization,” said Farmer, adding that she was recently able to provide data on a provider Prisma was hoping to recruit back to the health system. “I was able to quickly pull the financial numbers to support the request while we were sitting there. When we were using spreadsheets, I wouldn’t have been able to calculate that financial summary, especially not in just a moment’s time. It’s nice to be able to get that information quickly.”
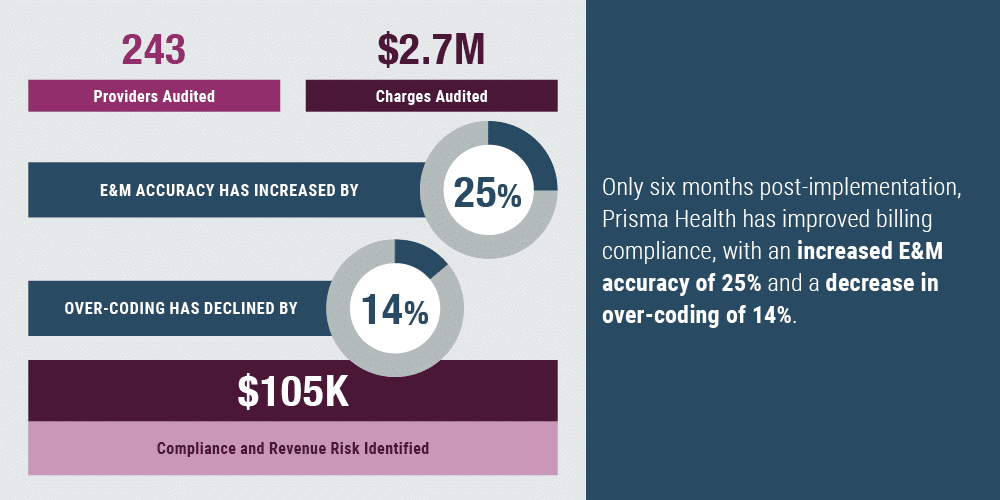
THE RESULTS
To download the full case study PDF, click here.