THE CUSTOMER PROFILE
A nonprofit health system operates as an integrated network spanning four states. The organization encompasses physician clinics, outpatient centers, and hospitals. The health system boasts an extensive infrastructure comprising 36K+ team members, supported by a network of 3K+ physicians, as of the close of 2022.
This nonprofit health system maintains a dedicated compliance team to support physicians and physician partners within their physician network, with a separate team overseeing compliance matters for the hospital and facility settings. The physician network compliance department is comprised of three specialized teams: compliance auditors who proactively review physicians’ documentation and billing, compliance liaisons providing as-needed risk-based provider education and support, and compliance consultants offering more specialized proactive, in-depth audits and operational oversight. The department is led by a Director of Compliance and an Assistant Director of Compliance.
THE CHALLENGE
Limited access to audit data, manual billing audit processes, and data inefficiencies impede timely decision-making and risk mitigation.
The three teams within the physician network compliance department faced significant challenges in evaluating and managing compliance risks due to a lack of tools for effective and efficient data management and analysis. They struggled with the inability to access audit data, the lack of the necessary tools to complete risk-based auditing, and the inefficiencies of manual audit processes – further complicating the overall compliance management process. As seen throughout the healthcare industry, work plans consistently outpaced available resources. Data manipulation was inefficient overall, and out of reach for many team members. Due to the complexity of the substantial workload, leaders found themselves entangled in numerous tasks, diverting their attention from more strategic leadership responsibilities.
Efficient access to audit data is crucial for the health system’s compliance team to enable timely decision-making, identify and mitigate risks promptly, and ensure adherence to regulatory requirements. It also supports ongoing performance monitoring, resource optimization, and accurate documentation for transparent reporting. The health network’s past audit data was distributed across disparate spreadsheets, preventing tracking, and trending over time, and making it more difficult to identify areas in which targeted education would be beneficial.
In addition to data access, automation, and analytic capabilities are crucial for accuracy, speed, and the ability to handle the complexities of billing audits, ensuring compliance while freeing up teams to focus on more strategic and impactful tasks. Manual billing audit processes in the health system introduced inefficiencies, increased the likelihood of errors, and consumed valuable time and resources.
One longstanding issue was the persistent inability to identify and report on providers whose E&M Bell Curve deviated significantly from others. Despite being on the department’s work plan for years, internal data limitations posed a substantial barrier, preventing the extraction of data at a granular level for insightful analysis. While the team could access the CMS normative curve data, gathering provider information required manual manipulations that the revenue cycle team exported from Epic.
“Our old system was convoluted and did not allow providers to see how they compared to their peers,” said the Assistant Director of Compliance. “It was always a question, but not something we were able to answer,” agreed the Director of Compliance.
THE SOLUTION
MDaudit provides efficient access to audit data, automates, enhances analytic capabilities, and streamlines manual billing audit processes.
Identifying and addressing billing compliance risks is crucial for protecting the financial stability of health systems by preventing revenue loss due to billing errors or non-compliance. Timely detection and resolution of compliance issues contribute to a proactive and preventative approach, reducing the likelihood of recurring problems and promoting a culture of continuous improvement. By streamlining audit processes and automating data analysis, healthcare organizations can allocate resources more effectively, allowing staff to focus on strategic initiatives and providing higher-quality patient care.
MDaudit has been instrumental in evolving the health system’s approach to identifying and addressing billing risks with robust tools to navigate billing complexities, fostering a proactive and effective strategy for ensuring regulatory compliance and financial integrity. With insights into over 300 audited billing risks per month, the platform provides a comprehensive view, enabling the health system to proactively manage compliance issues. A dedicated audit team leveraging MDaudit’s automation capabilities ensures efficient and thorough examinations of billing activities. Notably, the platform allows the health system to tie a financial impact to providers deviating from the E&M Bell Curve, providing a tangible metric for assessing non-compliant billing practices.
The health system’s successful implementation of MDaudit is largely attributed to robust change management strategies, skillfully guiding users toward a common goal. Together, the teams defined a clear vision of desired system functionalities and strategic prioritization of implementation phases. As the onboarding progressed, the teams demonstrated flexibility and a willingness to iterate, allowing for adjustments at key inflection points and ensuring long-term success.
Today, the health system’s compliance team overcomes data inefficiencies, enabling timely decision-making and risk mitigation. Unlike the traditional approach in many health systems, where obtaining data involves a cumbersome process of placing tickets or hiring a data analyst to navigate reports from the EHR or other systems, MDaudit streamlines data accessibility by empowering any authorized user to easily retrieve the necessary data without the need for data analysts or data experts.
An important example is the health system’s compliance department’s use of the MDaudit procedure utilization functionality to immediately answer questions and run ad hoc analysis reports. “That used to take so much effort. We had to put in a ticket with our revenue cycle department to request data. But like everyone else, their resources are limited, and they can’t always run reports right away, and then we would have to schedule another meeting to review the results once we received them. Using MDaudit, we can access the information we need in real-time” says the health system’s Director of Compliance.
MDaudit’s easier access to data also allows the compliance team to address inquiries from operational leadership more effectively. Historically, responding to questions about physician behavior and compensation involved labor-intensive processes, including the creation of provider profiles in spreadsheets based on complex data. With MDaudit, this workflow has been streamlined and automated.
The Assistant Director of Compliance describes, “Historically provider profiles were a large burden and primarily fell to me because of how complicated the process was. It could take weeks or sometimes up to a month, depending on the number of providers, to generate these profiles for operational leadership. One of the first things we worked on when we onboarded into MDaudit was building those profiles into the system.” What once took a month of the Assistant Director’s time can now be done in less than five minutes by anyone on the team.
The health system’s compliance leaders are responsible for ensuring regulatory compliance, optimizing resources, maintaining data accuracy, facilitating proactive decision-making, and fostering a work environment that is less burdened and more focused on the organization’s strategic priorities. MDaudit’s combination of effectiveness and efficiency empowers the health system to make proactive, strategic decisions while reducing the overall workload and stress on the team, fostering a more focused and confident approach to compliance management and operational tasks.
“We’ve been able to streamline processes for all our work streams. To make life easier,” says the Director of Compliance. “The effectiveness, the efficiency, the confidence that we can have in the results that come out of MDaudit have been vital. There hasn’t been a question that’s been asked from our compliance leaders or operational leaders that MDaudit hasn’t been able to answer.”
OUTCOMES
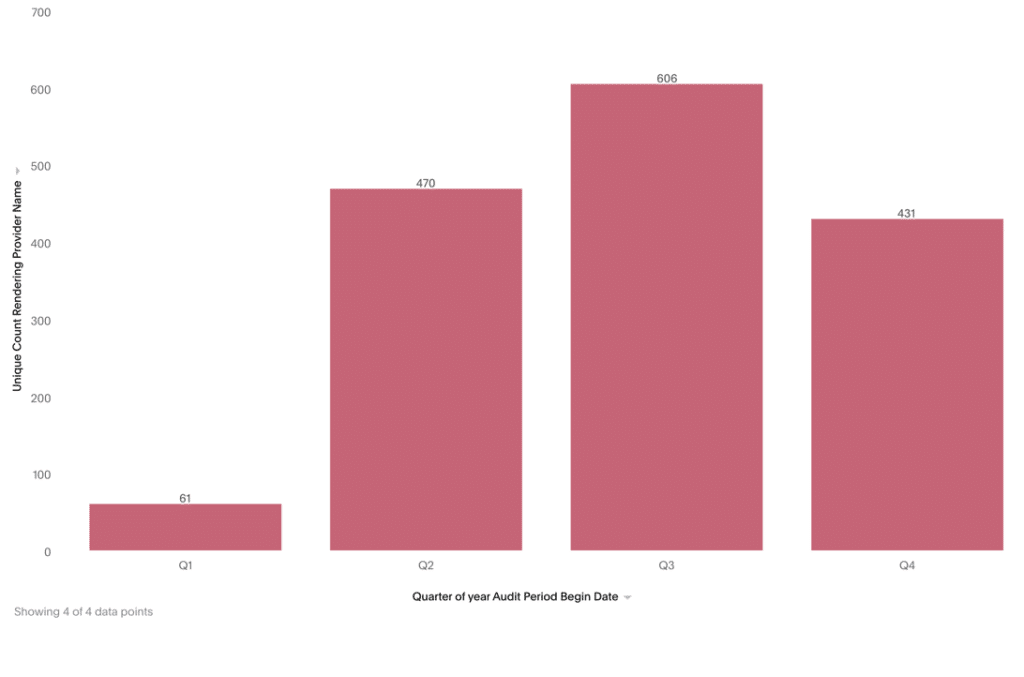
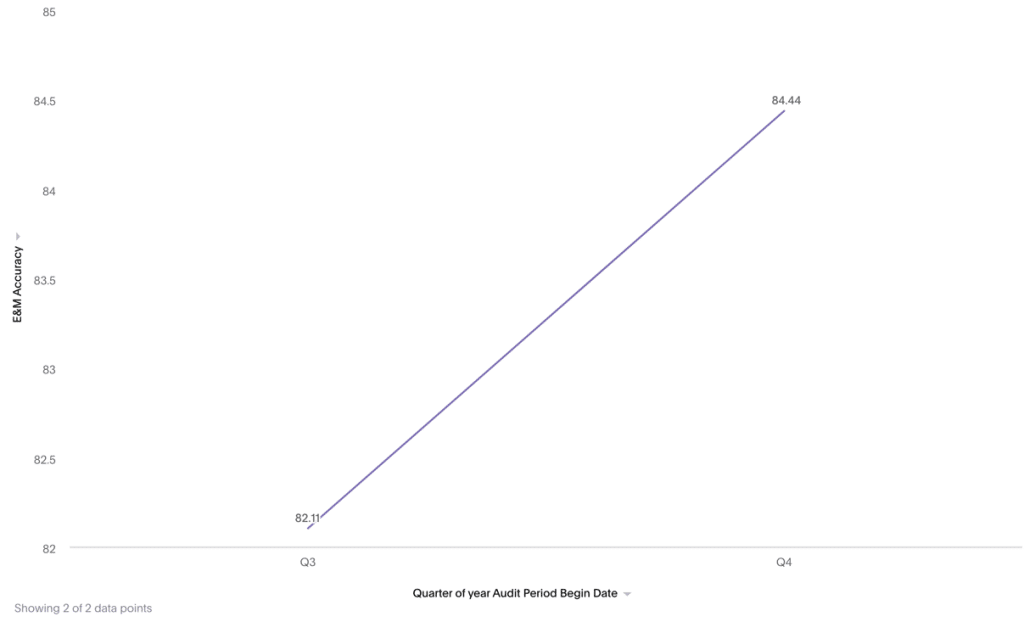
With MDaudit, approximately $6M of annual charges and 1500+ providers were audited in the first 12 months resulting in higher productivity, revenue capture, and risk mitigation. 10% of the providers failed their audits, and education was provided. The E&M accuracy incrementally improved through H2’2023 with a 2%+ net increase within the audited sample as a result of enhanced provider education. The health system is continuously increasing the scale of providers in their audited sample to assess more risks.
Annual Charges Audited with MDaudit
Annual Providers Audited with MDaudit
2% increase in E&M accuracy between Q3 and Q4 2023