THE CUSTOMER PROFILE
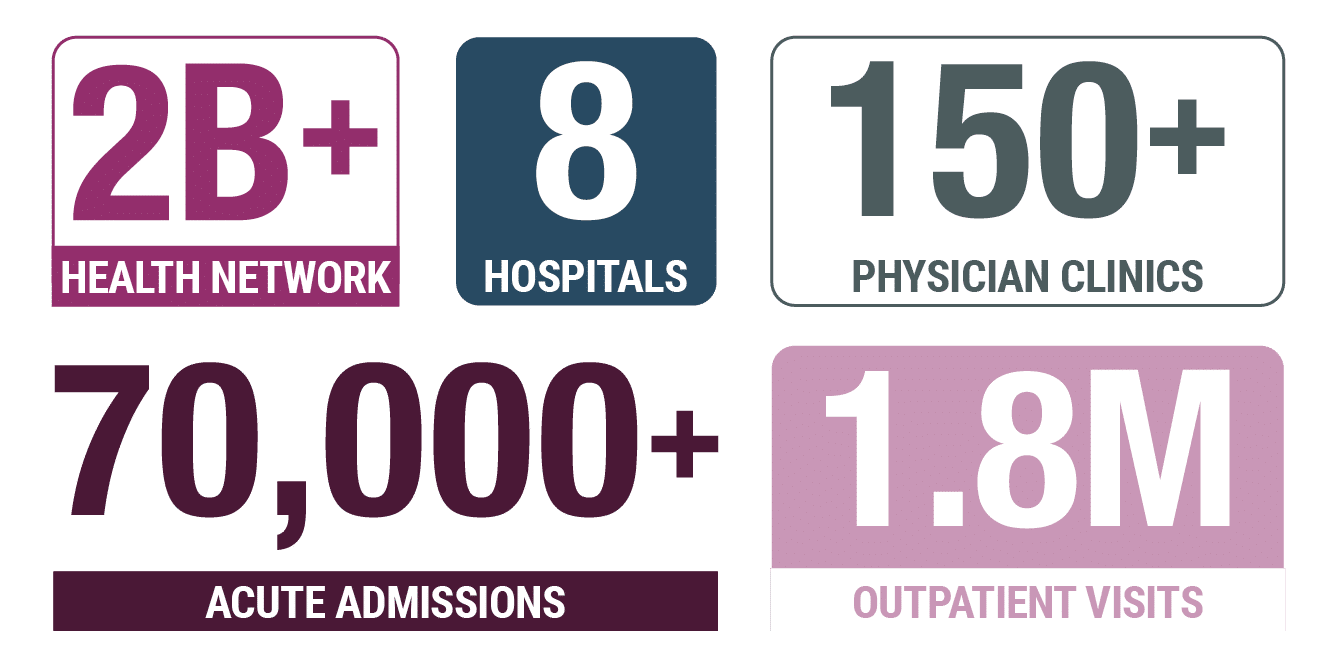
This faith-based, non-profit healthcare organization remains dedicated to the same critical mission upon which it was founded–delivering consistently positive patient outcomes while improving the community’s overall health and wellness. The health system, based in the western part of the U.S., operates several highly acclaimed hospitals and medical centers across multiple states. Compassionate and forward-thinking, this healthcare system offers a full spectrum of services from addiction treatment and trauma care to oncology, neuroscience, and obstetrics, as well as clinical trials and financial assistance for those who can’t afford care.
THE CHALLENGE
Rapidly changing regulatory requirements call for adaptive auditing workflows.
Changes in the healthcare industry are putting more pressure on oversight responsibilities for hospitals and health systems. To avoid financial penalties, reimbursement paybacks, and tarnished reputations, organizations need proven partners that they can trust.
An MDaudit customer and beta tester since 2015, the health system transitioned to MDaudit Enterprise in 2018. “We have had a very good partnership from the beginning,” says the system compliance officer. “We feel that partnering is an excellent way to get a product that is going to be functional for the way we want to use it, and I think that has served us very well.”
The billing compliance team recognizes that a healthy revenue cycle starts long before billing. From admissions to chargemaster creation and coding to scrubbing and submitting claims, optimizing revenue and billing compliance requires risk identification and mitigation throughout the cycle. The team routinely develops compliance work plans based on the organization’s risk factors and the current environment, taking into account areas of scrutiny from the Office of Inspector General (OIG), Centers for Medicare and Medicaid Services (CMS),the U.S. Department of Justice (DOJ), and the State Regulatory environment. Changes stemming from the COVID-19 pandemic were anything but routine.
Rapidly changing requirements for COVID-19 created new risks for healthcare organizations. Industry-wide, providers experienced high rates of denials, significant delays in payment, and a very high level of scrutiny from payers during a time of really great uncertainty. “We had to have a way to keep up with those regulatory changes from a monitoring perspective, to make sure that we were reporting everything–the codes, modifiers, and conditions codes–accurately based on the regulatory changes,” explains the system compliance officer. “Based on the Cares Act, CMS 1135 Blanket waivers, the Acute Hospital Care at Home initiative, and the state waivers, with everything happening at the time, we developed a new work plan. A COVID work plan to address our highest risks.”
As telehealth, lab, and condition code guidelines continuously changed, for example, communication across the health systems regarding the updates sometimes lagged behind their implementation. The compliance team used MDaudit to conduct rapid probe audits and rebill when necessary, protecting the organization from preventable payment delays or denials. MDaudit also allowed the group to continue monitoring error rates, ensuring crucial KPIs were met.
“Historically with any process, you have a workflow set up and people who understand what they need to do. With this sudden change, it was much harder because it was all new,” says the system compliance officer. “And there was a huge risk in COVID-19-related billing because the OIG and CMS said there was a risk. They said ‘We will be auditing these, make sure you do it right.’ So we needed to be able to structure a program to monitor, based on what we were required to do.”
There was a huge risk in COVID-19-related billing because the OIG and CMS said there was a risk. They said ‘We will be auditing these, make sure you do it right.’ So we needed to be able to structure a program to monitor, based on what we were required to do.
With MDaudit, the good news is that this is never-ending. You can continue to improve, improve, improve, improve because you’ve got this platform that you can do that with.
THE SOLUTION
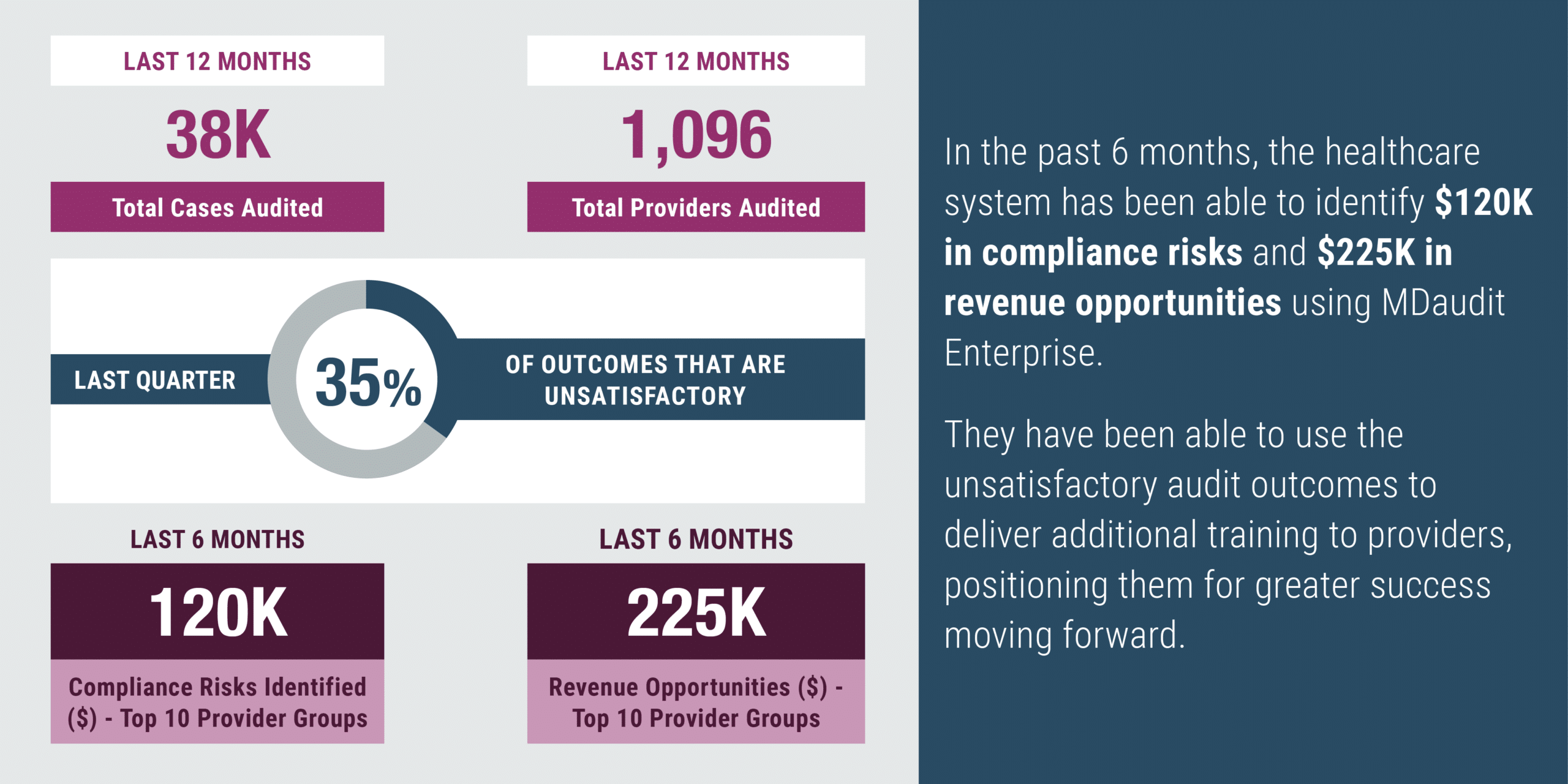
With MDaudit Enterprise, the organization was able to respond to known compliance issues, create a revenue cycle monitoring plan, and demonstrate value.
MDaudit uses claims and remittance data to help hospitals and health systems identify areas of risk and prioritize billing compliance resources to address them. “You cannot look at everything. We all know that and sometimes you don’t know what you just don’t know,” adds the system compliance officer. “We’re still seeing constant changes in coding and regulations — it’s astonishing how much it continues to change.” But MDaudit’s adaptability and responsive customer success team enabled the group to follow its compliance plans throughout this emergency and beyond.
The healthcare group’s COVID-19 work plan was to measure, audit, benchmark, make a plan to improve, and then monitor. “I think we were very successful in what we looked at. Our compliance plan was successful as it was set.” This clearly defined workflow structure will continue to serve the organization, long after the COVID-19 public health emergency (PHE) is over. The system compliance officer believes that when the PHE is pulled back, MDaudit’s systematic auditing workflows and monitoring will once again be a crucial part of the organization’s approach to ensuring coding is rolled back correctly amid changing regulations.
When the health system began using MDaudit in 2015, its use was limited to professional billing and internal audit workflows, “and they loved it,” says the system compliance officer. “Honestly, there’s more risk on the hospital side than there is on the professional side. There’s more risk, there are more dollars at stake. And you need to have a way to monitor that.” With MDaudit, the organization was able to monitor known compliance issues, create a revenue cycle monitoring plan, and report findings.
Implementation of MDaudit Enterprise also increased efficiency by making the reporting process faster. The system compliance officer states that “the interface is easier, it gets more user-friendly every day.” They point to enhanced functionality like the Revenue Optimizer module, audit insights, and analytics. “We really are starting to use the analytics side of that to track how we’re doing and it’s really been really helpful.”
“The real priority is taking care of patients”, describes the system compliance officer. “How do you support the caregivers so that they don’t have to worry about these things?” With MDaudit, “the good news is that this is never-ending. You can continue to improve, improve, improve, improve because you’ve got this platform that you can do that with.”
THE RESULTS
To download the full case study PDF, click here.