THE CUSTOMER PROFILE
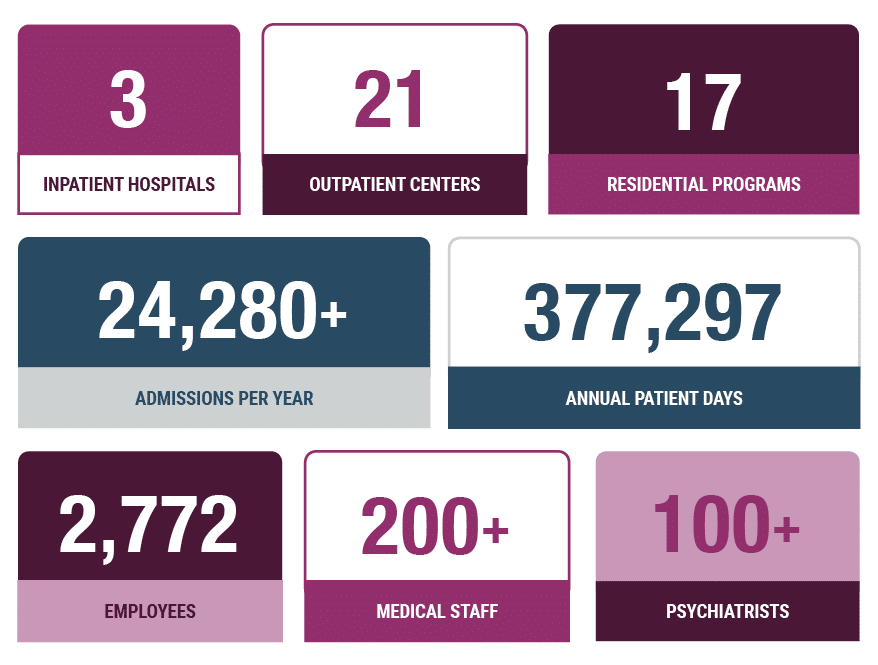
Now in operation for more than 115 years, Rogers Behavior Health is one of the country’s largest private, not-for-profit mental health and addiction services providers. With more than 2,700 employees and locations in 10 states, Roger’s multidisciplinary teams treat an average of nearly 1,500 patients per day and a total of 375,000 patient days per year.
The behavioral health system includes three inpatient hospitals and numerous outpatient centers and residential programs throughout a growing network of communities. Rogers treats adults, children, and adolescents with depression and other mood disorders, eating disorders, addiction, obsessive-compulsive and anxiety disorders, and posttraumatic stress disorder – regardless of their ability to pay.
THE CHALLENGE
To support its launch, the new compliance department required the most efficient, comprehensive platform.
For Rogers Behavioral Health, establishing a robust compliance department helps to protect the health system, its providers, and its revenue. Because much of the revenue is returned to patients by the Rogers Behavioral Health Foundation, protecting Rogers’ revenue means protecting its patient-focused mission to provide mental health and addiction treatment services.
In June of 2021, Sharon Moehle was hired to create and direct a billing and coding documentation auditing department – the first at Rogers Behavioral Health. She brought on a team of five auditors, developed an audit work plan that includes facilities and professional fees audits, and set out to find a technology platform to empower the team and their audit plan.
“I looked at dozens of software companies. A lot of them were okay for E&M audits, but they didn’t have all of the features we needed,” said Moehle. “MDaudit was superior to the other auditing programs I saw out there.”
At a previous employer, Moehle used an auditing system that required data to be exported to spreadsheets for reporting, which created a great deal of extra work. Amid ramping up a new department and establishing relationships within the new team and across the organization, Moehle’s group did not have time for extra work. The new software system would have to be user-friendly, efficient, and comprehensive.
“It was really important to me to be able to run the reports that I need, and to have customer service available to help me when I need it. MDaudit has the best customer service that went along with the excellent software,” she explained.
Moehle acknowledges that new technologies always have a learning curve and come with questions, but “MDaudit had our back through implementation and training. Now we’re really gaining momentum and experience.”
It was really important to me to be able to run the reports that I need and to have customer service available to help me when I need it. MDaudit has the best customer service that went along with the excellent software.
The greatest value that MDaudit brings is the ease of putting the audit data into a system and then getting reports out. That is huge.
THE SOLUTION
MDaudit audit workflows and reporting offer time savings and confidence.
Less than 18 months after implementing MDaudit, the Rogers Behavioral Health billing compliance department offers comprehensive auditing and education to its providers. “My number one goal was to get our providers audited and educated, and we did that within the first four months of our department’s inception,” says Moehle. Supported by reports from MDaudit, each provider audit is accompanied by the rationale, education, and tools to improve coding in the future. “One of our strategic goals for this year ahead is to get all of our providers to an overall accuracy of 93%, and I believe we can make that, too.”
Auditing aides such as E&M and risk area worksheets offer flexible approaches to meet the needs of specialty providers. For behavioral health providers, such as Rogers, MDaudit includes inpatient and outpatient E&M resources, worksheets for psych evaluations, and more. “We can even create custom risk area worksheets for whatever we need, but it was already there, so we didn’t have to do that,” says Moehle.
Because users can run their own reports without submitting requests to IT or other departments to download information from EHR or RCM systems, MDaudit offers significant time savings and the confidence that reports reflect the correct information. “The greatest value that MDaudit brings is the ease of putting the audit data into a system and then getting reports out,” describes Moehle. “We have the ability to run ad hoc reports like billing trends and audit insights. That is huge.”
Recently, the Rogers compliance department received an educational letter from a payer that identified concerns that the billing for a Rogers provider was out of range compared to their peers. Moehle’s team was able to identify all Rogers providers who were billing specific codes and audit them to ensure that their documentation supported their billing. They then used the MDaudit bell curve reports to compare their providers to one another and to other behavioral health providers nationally.
“It was a very handy timesaver to have those bell curve numbers within MDaudit,” explains Moehle. “But it was also a great example of why it’s important to have the confidence that the information we are sharing across the organization is comprehensive and accurate.”
THE RESULTS
To download the full case study PDF, click here.