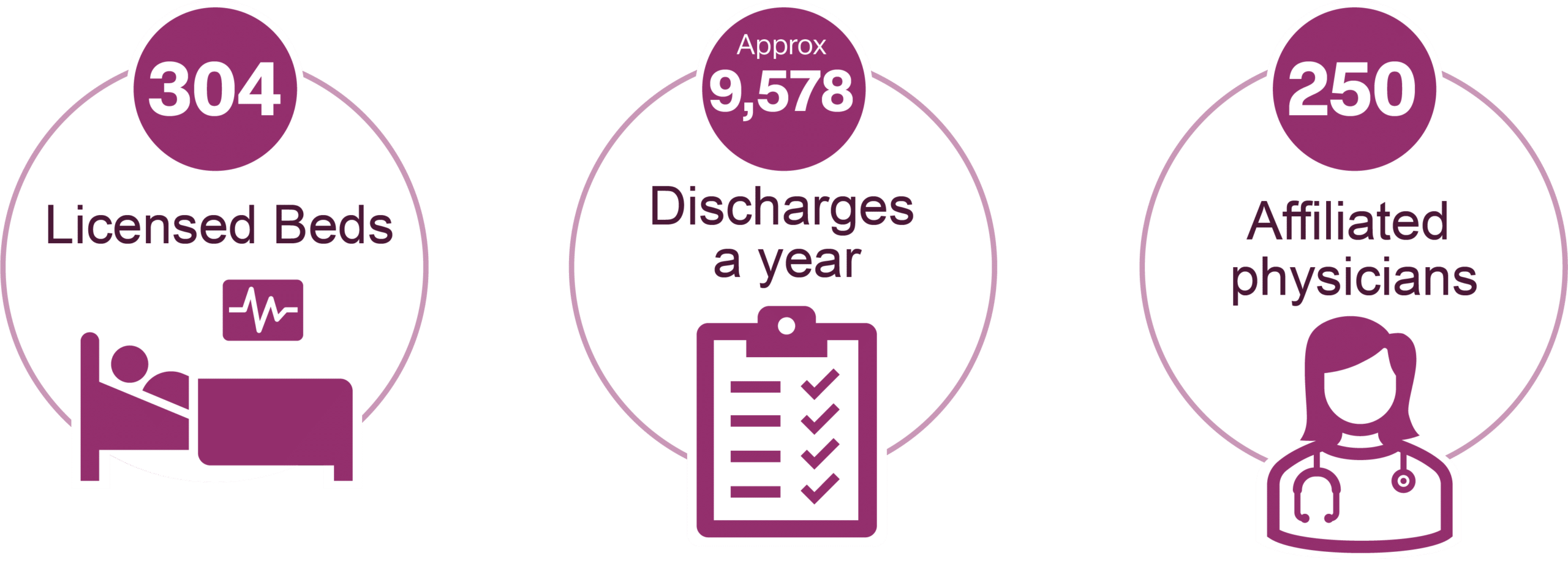
THE CUSTOMER PROFILE
A 304-bed community hospital located in the Southeast, offers cardiopulmonary care, cancer care, radiology, women’s health, and laboratory services to area communities. As part of its operations, it features satellite clinics devoted to family care, diagnostic imaging, occupational health services, and outpatient rehabilitation.
THE CHALLENGE
Unkept promises, no training, and hidden fees made the cheaper solution, the more costly option.
In 2015, the aforementioned hospital was manually creating bell curves to compare their providers’ E & M codes to national averages, a quarterly task that took a week and a half to complete. To create organizational efficiencies and reduce risk for the organization, the CFO tasked the compliance team with identifying and implementing a system to automate the process. The team selected another auditing program based on its impressive demo and affordable price but discovered almost immediately that they had not gotten what they paid for.
“We did not receive any training from the other vendor. It was just sort of like, ‘Here’s your product, good luck.’ We just had to teach ourselves,” recalls the clinical documentation and coding compliance supervisor. “We never received all the bells and whistles we were demoed. We basically just got the audit tool, even though I was constantly calling them about the other things that we had purchased.”
After years of discussions and requests that yielded no results, they offered the vendor one last chance before replacing their software, but were told that it would cost an additional $10k to import claims data into their system to create the bell curves – which was the main reason they initially made the purchase.
The clinical documentation and coding compliance supervisor recalled a previous conversation with a colleague who recommended MDaudit, sharing that the platform was data-driven and came with a dedicated customer success team who ensured it could interface directly with her EHR system. Most impressive, though, were the reports she could create in MDaudit – reports unavailable in the other auditing solution provider’s system. At the time, she expected such a robust solution would be too expensive for her small hospital. Still, ultimately the leadership team determined that the value MDaudit would deliver to the organization made it a worthwhile investment. She said the hospital CFO agreed, “if it is going to help identify lost revenue, gain better control of our denials, produce the bell curves, and get our compliance program in better alignment, let’s do it.”
You’re only as good as the product you are working with. And if the product won’t do what you feel like it needs to do, then you’re handicapped. In this day and time, there’s no time to find a workaround. You’ve got to be able to work efficiently.
THE SOLUTION
MDaudit delivers true value with system integration, automated workflows, intuitive reporting, and a dedicated customer success team.
With the truly integrated MDaudit billing compliance and revenue integrity platform, the hospital’s compliance team can run their bell curves and much more – with no time wasted manually importing spreadsheets to access claims data and analytics. MDaudit has perfected the data ingestion process to deliver a uniquely seamless experience like no other system.
“MDaudit pulls in all of our claim information. We don’t have to worry about adding demographic information at all; it is all right there. The automation helps tremendously and has saved us a lot of time,” says the clinical documentation and coding compliance supervisor. “To be able to tap into our own data and understand and use it has been very valuable.”
MDaudit has invested significant development resources refining its industry-leading analytics. Users can easily identify at-risk provider populations and billing trends using daily claims data. Effectively addressing undercoders, overcoders, and trends outside normative ranges can protect hospital revenues. “We started out by working with our overcoders and undercoders. It was so exciting to see in our reports that a specific undercoder was improving from month to month. It was a game-changer for us to be able to see her improvement as the fruit of our labor,” she recalls . “And those improvements mean improvements for the organization’s bottom line, too.”
She explained: “You’re only as good as the product that you’re working with. And if the product won’t do what you feel like it needs to do, then you’re handicapped. In this day and time, there’s no time to find a workaround. You’ve got to be able to work efficiently.”
At MDaudit, a dedicated customer success manager works alongside the client’s team every step of the way to maximize meaningful value. The dedicated customer success manager knows what’s in the contract, learns the organization’s unique audit program, and provides the training and support to ensure the system can be used the way it was intended when the contract was signed.
More recently, this hospital has begun leveraging MDaudit to address the millions of dollars in previously unchecked denials. They noted they had mistakenly been led to believe that there were not a significant number of denials related to prior authorizations and that the majority were coming from medical necessity issues. However, with MDaudit, the compliance team could identify the source of their denials and work directly with the precertification team, sharing data from MDaudit regularly and working together to understand and eliminate barriers to proper precertifications to reduce denials and increase revenues.
MDaudit delivers additional operational efficiencies with functionality for users across the entire organization in one common system. For example, with their clinics under new management, the hospital has added five new directors. MDaudit has enabled the compliance team to share information with them, highlighting where denials are problem areas in their clinics and how it’s financially affecting the entire organization.
While many vendors force organizations to adapt audit and compliance programs to their software workflows, the MDaudit platform offers users the flexibility to run programs as they best fit the organization – from prospective and retrospective audits to reviewing denials and built-in analytic insights. Based upon the understanding that no two healthcare organizations are the same, MDaudit was designed for all organizations. Whether it’s 10 providers or 10,000, MDaudit scales to meet needs regardless of size.
Looking ahead, the hospital’s team has begun to leverage the advanced features of MDaudit to expand their compliance program. Though they have traditionally focused only on E&M coding, they are now identifying new areas of opportunity for improvement. Audits for surgeries, or office visits and procedures billed for the same day, for example, were not possible prior to MDaudit. Adding prospective audits and working closely with the Revenue Cycle Director and the Director of Health Information Management to evaluate trends on a facility-basis are also on the roadmap.
“I just don’t see that it has a limit. As long as we’ve got a claim in the system, I think that we should be able to pull any kind of data that’s needed. I don’t see any limitation to it,” she says.
THE RESULTS
For Q2 2021 – Q4 2021: