“If it isn’t documented, it didn’t happen.” That’s the familiar mantra of the healthcare industry. But simply documenting a patient encounter isn’t enough. The patient care must be documented properly, or the negative financial implications can be significant.
That’s why many healthcare organizations have embraced Clinical Documentation Improvement (CDI) programs to enhance their revenue integrity efforts. The results of these initiatives have been dramatic. Nine out of ten hospitals with more than 150 beds have seen increases of more than $2 million in valid revenue and reimbursements as a result of a dedicated CDI program.[1]
One of the greatest benefits of proper clinical documentation is the impact it has on an organization’s Case Mix Index (CMI) – an important financial indicator that directly impacts a hospital’s finances.
What is Case Mix Index and why is it important?
CMI is a metric that the Centers for Medicare and Medicaid Services (CMS) uses to assess the mixture, clinical complexity, and resource needs of all patients treated in the hospital. It reflects the average relative DRG weight of a hospital’s inpatient discharges. The CMI is calculated by summing Medicare Severity-Diagnosis Related Group (MS-DRG) weight for each discharge and dividing the total by the number of discharges.
A higher CMI means more reimbursement dollars for providing care because it indicates a hospital is treating a sicker patient population. CMI is the foundation for the methodology by which a healthcare organization received payment from CMS.[2]
Since a high CMI indicates a more complex and resource-intensive case load (resulting in a higher reimbursement rate), there must be corresponding clinical documentation in place to support these types of cases. Without this proof, the CMI would be lowered and negatively impact the amount of reimbursement to which an organization is legitimately entitled.
Improving clinical documentation to validate a higher Case Mix Index has proven to be an effective way to increase an organization’s legitimate revenue. An example of one such organization is Summit Healthcare Regional Medical Center in Arizona. Following an initiative focus on improved documentation, they reported a 20% increase to their CMI involving complications and comorbidities and realized nearly $600K in additional revenue in a matter of months.[3] Eighty-eight percent of hospitals have documented quality improvements and increases in CMI within six months of beginning a Clinical Documentation Improvement initiative.[4]
Data analytics are key to improving CMI
Improving documentation that leads to higher CMI begins with a program that encompasses a comprehensive analysis of an organization’s coding and billing data. There are two main ways that data analytics can lead to improved CMI accuracy: continuous monitoring and benchmarking.
1. Continuous monitoring
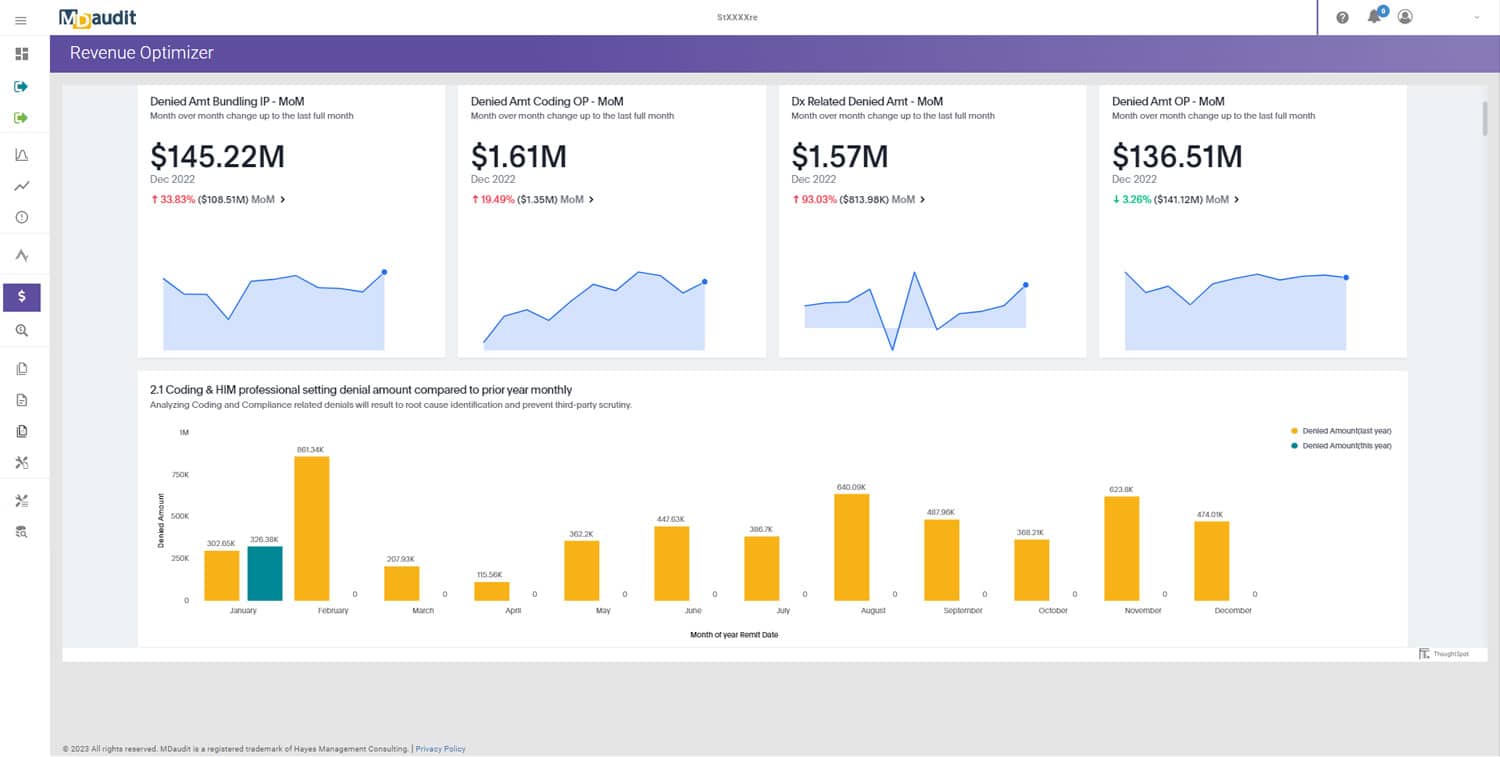
To ensure proper coding and documentation, an organization must monitor coding activity and claim accuracy on an ongoing base. This allows billing compliance, HIM, coding and revenue cycle leaders to track trends, detect anomalies, identify the root cause, and implement corrective action to make sure the same errors do not reoccur.
Many organizations rely on periodic chart reviews to audit their clinical documentation. This method is both risky and expensive. Reviewing random cases for documentation errors 2-4 times a year may waste precious resources on coders who are performing well while risking overlooking those who are doing poorly.
Chart reviews are also expensive. For example, the American Medical Foundation Patient Safety Organization requires an upfront charge of $1,000 to cover administration costs, $350 per hour for individual reviewers conducting the chart analysis and writing reports, and $350 per hour or more for onsite visits depending on the specialty.[5]
Alternatively, by leveraging auditing software that enables continuous monitoring of key DRG codes – such as the MDaudit Enterprise – you are able to immediately uncover the direction and magnitude of potentially negative trends. This allows you to focus your investigations on problem documentation areas and initiate immediate corrective action.
2. Benchmarking
Tracking and analyzing your own clinical documentation quality metrics/KPIs is important in determining that clinical engagements are being captured accurately. But it is just as important to compare your internal metrics with a cohort of similar organizations.
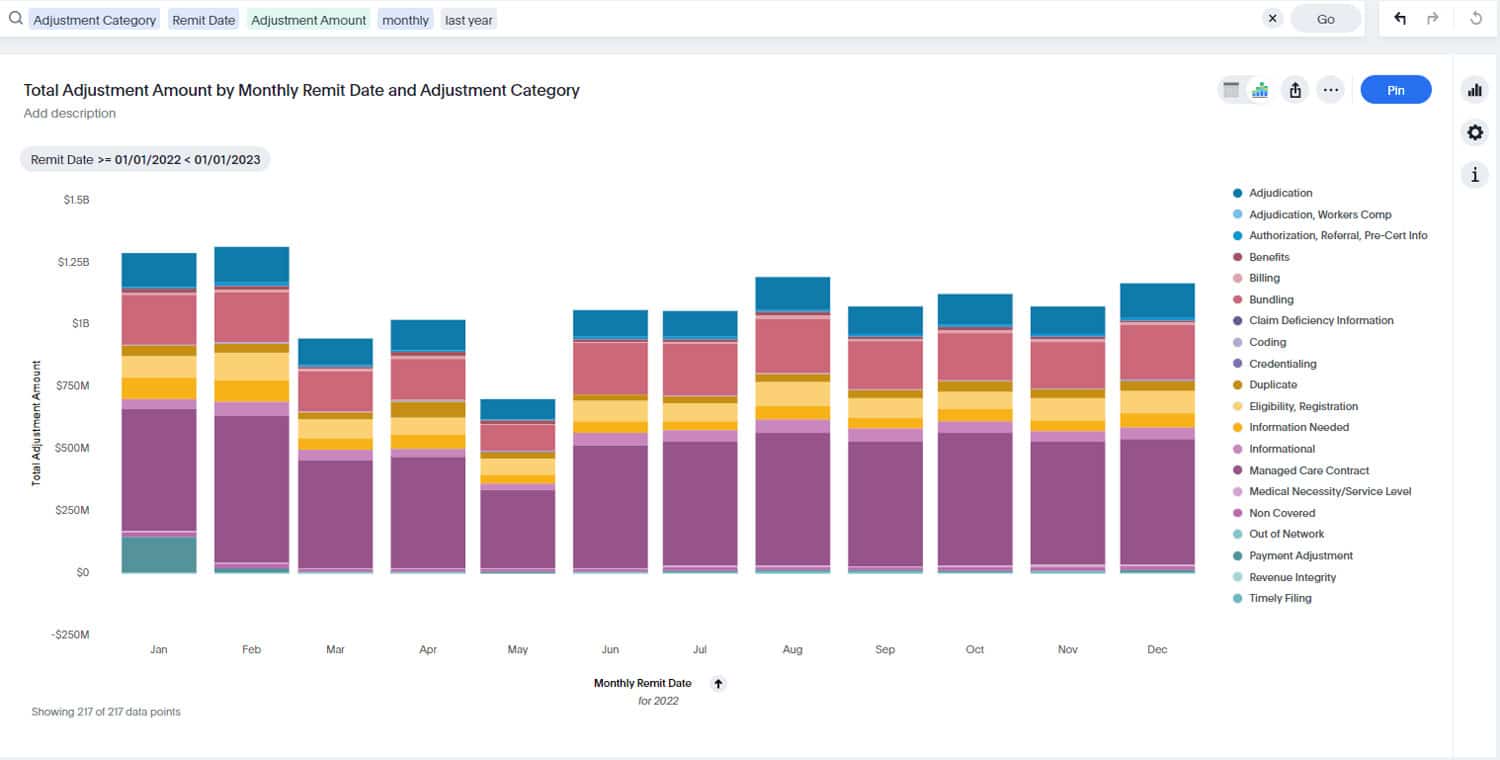
Benchmarking your performance relative to your peers allows you to compare specific DRG reporting with other hospitals, and can help identify areas where you may not be measuring up. This type of comparative analysis is another way to highlight where your documentation may be lacking and negatively impacting the accuracy of your CMI. The MDaudit metric card shown above shows the peer benchmark range for Surgical DRGs for CCs/MCCS, allowing you to assess your organization’s performance on this metric relative to similar organizations.
As pressure on revenue and profit margins continues to grow, it’s essential to ensure that you are capturing all the legitimate revenue to which you are entitled. Having the correct CMS reimbursement rate – based on an accurate CMI – is critical to making that happen. You can ensure you have the appropriate CMI by leveraging the right software tools to continuously monitor activity and compare results with peer organizations.
[1] 93% of Healthcare Execs Seeking Improved Data Analytics, CDI, by Jennifer Bresnick, HealthIT Analytics, October 22, 2018.
[2] Ther Revenue-Threatening Link Between CMI and DRG Shifts, Laurie A. McBrierty, MLT, ASCP, Career Step
[3] Maximizing Revenue Through Clinical Documentation Improvement, RevCycle Intelligence, October 7, 2017.
[4] 93% of Healthcare Execs Seeking Improved Data Analytics, CDI, by Jennifer Bresnick, HealthIT Analytics, October 22, 2018.
[5] American Medical Foundation Patient Safety Organization website, accessed September 10, 2019