Telehealth, adjusting to the pandemic, and of course, MDaudit user stories and new enhancements were the hot topics at this year’s MDaudit User Group Meeting. This year we embarked on our first-ever virtual meeting which brought us a record-breaking number of attendees. Without the traditional financial and time barriers that come with a live multi-day meeting, more organizations and hundreds of people were able to participate this year.
Here were the biggest takeaways from this year’s meeting.
Organizations are looking to move the auditing process to be more real-time to speed up the receipt of payments.
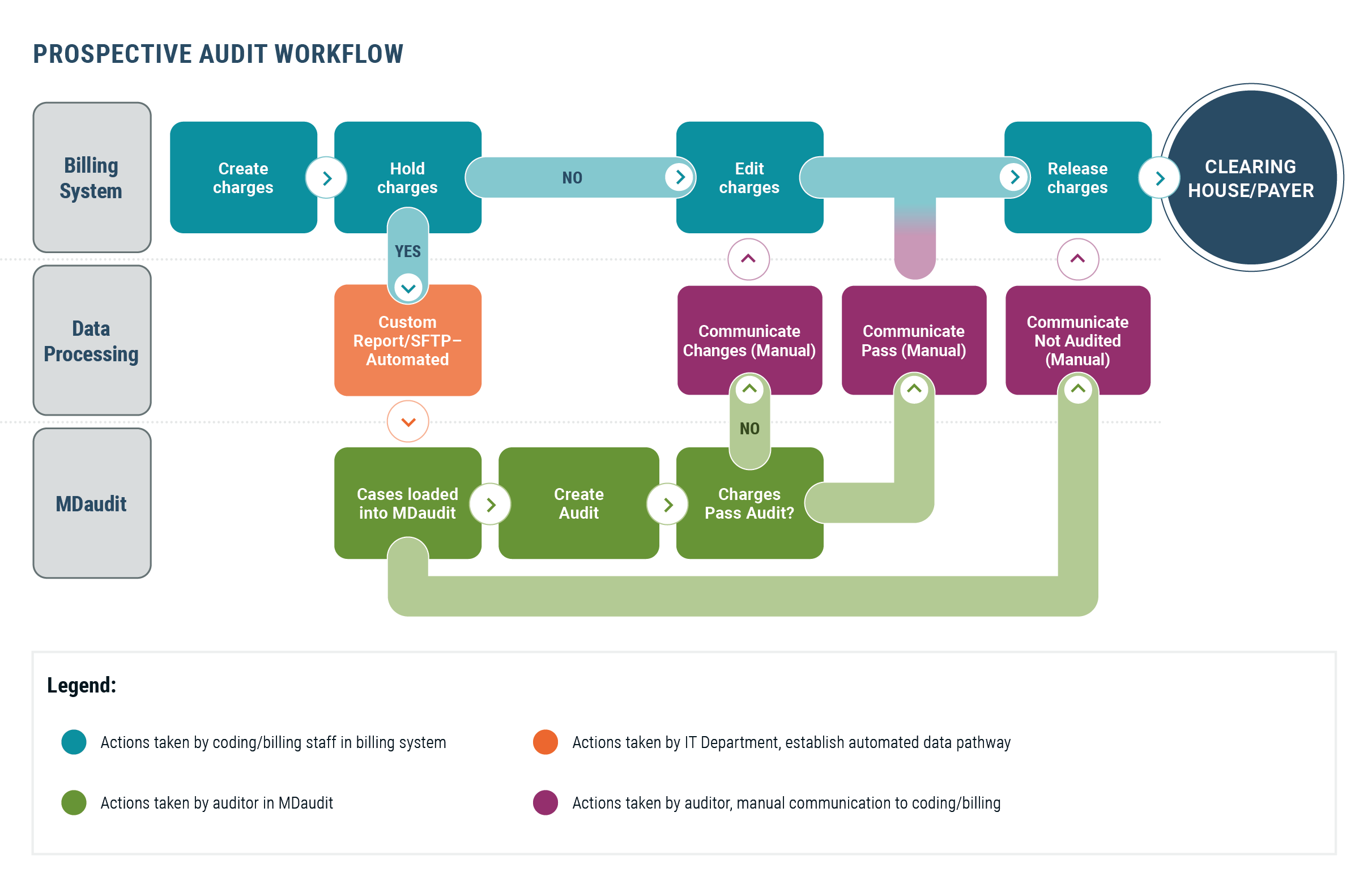
Peter Butler, CEO at Hayes, described the story of a client who called indicating she needed to start conducting audits before claim submission. Now, especially with COVID, she wanted to be more prospective (or proactive) with their audits by putting claims on hold so the auditors could dig in deep and make sure that the claims are coded appropriately before being sent to the payer.
This sentiment was echoed by clients during our Prospective Auditing session in which our product experts were able to illustrate how MDaudit Enterprise can help health systems and organizations review charges prior to submission. Not only is the first pass pay rate improved to accelerate revenue collection, but it also reduces the workload for those working potential denials.
There is increased use of risk-based auditing to enable smaller teams to conduct more meaningful audits, with limited resources.
A client on the East Coast shared with the group how her team uses MDaudit Enterprise to enable her small team to take a risk-based approach to audits – essentially, being able to do more with less.
Her three-person auditing team supports over 1400 physicians and mid-level providers with a wide variety of medical specialties. While the ideal ratio of providers to an auditor is 100, they have 480 providers per auditor. Given the size of their department, they are trying to use their time wisely and have shifted away from larger-scale audits and try to focus on potential risk-areas.
Before implementing MDaudit Enterprise, patterned issues would surface multiple times during routine audits however, without any trending capabilities the patterns were frequently missed. Then when they did see it, they would have to provide IT with the parameters to pull data based on the trend they were focusing on. This made monitoring difficult since we were dependent on the IT team and it was not real-time data.
Now, they have all the data at their fingertips and can use the MDaudit Enterprise dashboard to spot trends and focus on risk areas. They use the E&M Bell Curves to see who may be over-or-under-coding, conduct new provider audits, and focus on specific modifiers that are important to them.
Other clients are also leveraging MDaudit Enterprise to focus on particular risk areas within their audits. During the meeting, they demonstrated how they conduct new provider audits within MDaudit Enterprise along with showing how MDaudit was able to allow them to easily create audits focused on COVID-19 services.
Educating providers and coders is more challenging when your compliance team works remotely.
For compliance officers, COVID-19 has proven to be a challenge when it comes to face-to-face time with providers and the impact it has on providing education. The information auditors share is not being retained so they are not seeing the changes needed. Without being in the office, they are not being asked clarification questions that might prevent problems. And it will only get worse with all the new changes 2021 will bring.
- During our Chief Compliance Officer panel, many officers shared ideas with the group about how to be more effective in communicating and educating providers and staff.
- Use your technology. Connect with people online, use automation to get your message out, and use online education.
- Make your education session snappier, visually more interesting, and shorter.
- Setup virtual Q&A or Ask the Expert sessions and keep your web session open for hours at a time to allow people to jump on whenever they have a question.
- Have frequently asked questions on your website to make it easy for people to find the information they need.
- To help ensure education sticks, re-audit a provider within 30 days of their education session so you can talk to them if you are still finding problems.
Compliance Officers are concerned about external audits and scrutiny related to telemedicine.
The use of telehealth tools has skyrocketed since the pandemic, and while telehealth is giving patients a way to stay connected with their providers, it has kept the compliance teams on high alert. Providers are using the wrong tools to communicate, there is variability in requirements by state, and educating providers and coders on documentation requirements are only a few of the concerns we heard.
One of the key concerns we heard is the Office of the Inspector General (OIG)’s current focus on telemedicine. The OIG Criminal and Civil Enforcement page is filled with articles related to enforcement actions related to telemedicine fraud. In addition, the OIG workplan has multiple items related to the delivery of Medicare services via telehealth.
MDaudit Enterprise customers have been using the platform to conduct focused prospective and retrospective audits allowing them to target telehealth services to understand and mitigate risk.
There is more partnering between compliance and revenue cycle teams than ever before.
“Years ago, the compliance officer was just mitigating risk. They had no focus on revenue. Now, that is changing, and we see more organizations where there is a partnership between billing compliance and revenue integrity. They bring more people into the conversations and share what they are seeing to help the revenue cycle, not just mitigate risk.” Said Peter Butler, CEO, during the opening session.
Throughout the conference, and especially during our CCO panel, we heard tales of the compliance teams working together with revenue cycle and other teams through their organization to build stronger relationships. Revenue cycle teams are sharing concerns they see with their compliance teams and compliance is educating on revenue cycle when they can.
One of our clients in the south shared how the pandemic has given the compliance team the chance to increase transparency about what compliance does and how they can serve as a partner. They are sharing their workplan more widely and have expanded who they talk with about different risks to expand the scope of their audits. It is helping them create partnerships with many of the teams in their organization.
Plus, users were excited to see the latest and upcoming updates to MDaudit Enterprise.
Along with all the peer-leadership sessions, the user group meeting also showcased many new and upcoming features within MDaudit Enterprise. Earlier in the year we released a workflow for coder audits, this fall MDaudit Enterprise obtained their HITRUST CSF certification, and soon we will release our Audit Insights module.
Our new Revenue Optimizer was also a popular topic. Revenue Optimizer is a new data analysis tool that provides insights on the root cause of denials to help mitigate avoidable denials and maximize revenue. Clients participated in the demonstration during the meeting and shared how they find the most beneficial features to be the pinboards which simplifies complex data through visuals that make it easy to understand and drill down into specific data points.
Want to learn more about MDaudit Enterprise and how it can help your organization thrive? Request a demo today.