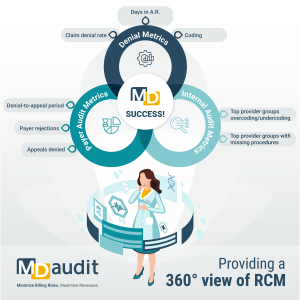
When healthcare organizations assess revenue integrity metrics, they often focus on denial metrics. While these are critical indicators of financial health, they only scratch the surface of true revenue integrity. At MDaudit, we advocate for a holistic revenue cycle management (RCM) approach. This approach requires a 360° view of the revenue cycle continuum. We create this view by incorporating internal audit metrics, payer audit insights, and denial trends to optimize revenue outcomes and mitigate compliance risks.
Expanding the Scope of Revenue Integrity Metrics
Denial Metrics are the traditional approach for assessing revenue integrity. They remain foundational to the revenue cycle by providing insights into denial rates, days in A/R, and the percentage of recoverable versus non-recoverable denials, providing visibility into inefficiencies and reimbursement bottlenecks. However, focusing solely on denials can result in a reactive rather than a proactive revenue integrity strategy.
Internal Audit Metrics: Identifying Root Causes
A proactive approach requires healthcare organizations to analyze internal audit metrics highlighting coding and documentation deficiencies before they lead to denials or payer audits. These metrics can include:
- Top provider groups undercoding or overcoding – Identifying trends that may indicate a need for provider education, process improvements, and corrective action plans (CAPs)
- Top provider groups missing procedures – Ensuring complete and accurate documentation to avoid lost revenue opportunities.
- Trends in modifier use and CPT/DRG code accuracy – Pinpointing inconsistencies that may trigger payer audits.
Payer Audit Metrics: Understanding External Risk
Payer audits are a significant financial and operational burden for healthcare organizations. Tracking payer audit metrics helps organizations anticipate risk and refine compliance efforts. Key insights include:
- Where ADRs are coming from
- Most frequently targeted procedures or specialties in payer audits.
- How much is being retained, and how much is being refunded – and why –.
- Common audit triggers to identify gaps in documentation or coding.
Leveraging Technology for Comprehensive Revenue Integrity
The complexity of revenue integrity requires data-driven automation and analytics to unify insights across internal audits, denial management, and payer audits. MDaudit’s platform enables healthcare organizations to:
- Monitor trends in real time across all revenue integrity metrics.
- Identify areas for provider education to prevent undercoding or overcoding.
- Optimize compliance strategies by proactively addressing risk areas before they lead to payer scrutiny.
These key focal points create a panoramic view of the revenue cycle continuum.
A Panoramic View
A holistic approach to revenue cycle management requires healthcare organizations to apply revenue integrity metrics effectively, helping their teams move beyond denial-focused strategies alone. By integrating denial metrics, internal audit data, and payer audit insights, organizations gain a 360° view of revenue cycle risk and opportunity—leading to better financial performance, fewer compliance risks, and stronger revenue outcomes across the continuum.
Ready to take a comprehensive approach to revenue integrity? Learn how MDaudit can help your organization stay ahead of compliance and financial risks.



