In this 7-part series, we will explore the tactics you can employ to build and optimize a revenue integrity team designed to create measurable value for your organization. You can find the first part here.
Revenue integrity is often described as a process of breaking down silos between billing compliance and revenue cycle to create a more holistic approach to revenue flow. One of the aspects of a successful revenue integrity strategy is performance measurement and benchmarking. While most organizations periodically review their billing performance, benchmarking offers the ability to compare charge patterns against other datasets. This helps you understand if performance is typical or follows an odd pattern that needs to be explored.
The benefits of benchmarking are:
- Identify risk of over/under coding or unusual patterns
- Find opportunity for improvement
- Share insights with leaders and providers
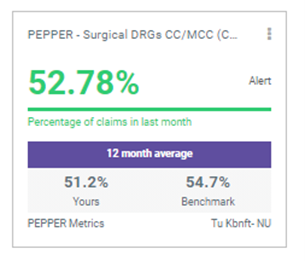
Even if you aren’t benchmarking your organization’s performance, CMS and commercial payors are. Consider Comparative Billing Reports (CBRs) and the Program for Evaluating Payment Patterns Electronic Reports (PEPPERs). The reports available to providers and organizations to help benchmark performance against specific measures.
There are a handful of different datasets hospitals and health systems typically use for benchmarking.
- Your own historical performance
- Other providers/procedures in your organization
- CMS national data
- Hayes customers have access MDaudit Cohort data
A properly structured analytic solution should allow you to benchmark by facility type, specialty and location type and should allow you to look at multiple measures providing much deep insights into billing patterns by providers or procedures you should explore further.
Once you find those discrepancies, start digging to understand the reason. In some cases, nothing is wrong at all and the pattern of your organization may just fall outside of the normal patterns. However, you may find that something may need to be addressed. Typically we find that when you start to slice the data by provider, coder or facility, you will start to find some outliers. A specific provider who is under- or over-coding. Or a new provider to your organization is coding differently that your other ones. Or maybe there is a shift in the type of patients and procedures being done.
Then, when you discover the root cause, you have the ability to make an impact. Is a provider undercoding? Educate them to so they are coding correctly which has a positive impact on your revenue. Is a coder coding incorrectly? Through education and prospective auditing, you can avoid compliance risk moving forward.
Next up in the series we will discuss using analytics to focus your efforts.