A staggering 82% of denials in 2022 were associated with Medicare, posing a serious threat to healthcare organizations’ revenues that is exacerbated by rapidly climbing third-party audit volume and declining patient visits. These were among the key findings of the 2023 MDaudit Annual Benchmark Report, an in-depth analysis of benchmarks and insights derived from more than 70,000 providers and 1,500+ facilities providing data to MDaudit for auditing and charge and denial analysis. Included in the analysis were $1.5 billion in professional and hospital claims audited and more than $100 billions of total charges denied by commercial and government payers.
The findings of the second annual auditing and revenue integrity report should be the push billing compliance leaders need to find more efficient ways to grow revenues in part by retaining at-risk revenues, including leveraging data and analytics as catalysts to proactively detect risks and perform audits for corrective action. Per the MDaudit analysis, data-driven, risk-based audits – which were up by 28% in 2022 – can complement the annual compliance plan to ensure effective audit scope coverage. Further, by continuing to deploy both retrospective and prospective audits, the latter of which was up by 31% in 2022, compliance teams can drive cross-functional initiatives that mitigate compliance and revenue risks.
Defending Revenues
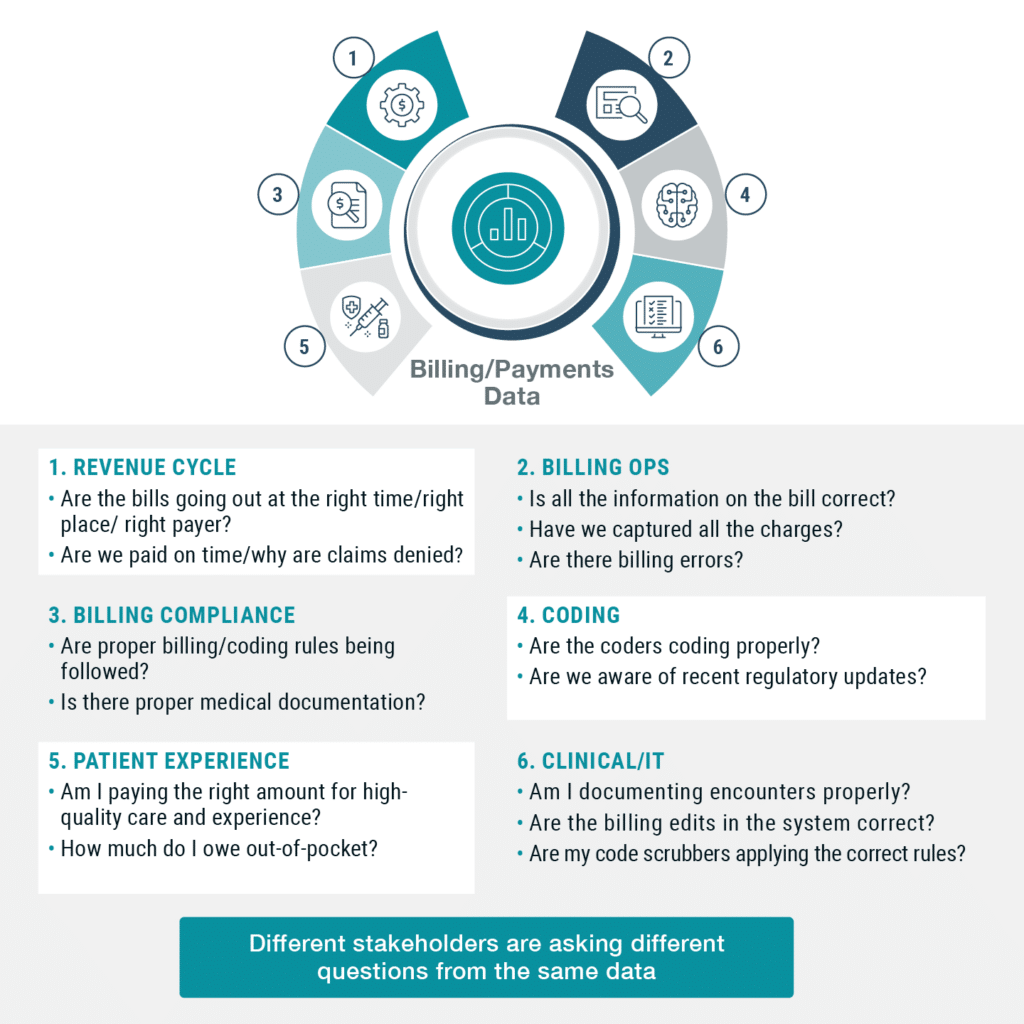
A key element of a successful revenue defense going into 2023 is to help compliance teams become more efficient in managing external payer audit requests to retain at-risk revenues beyond their internal auditing workplan and strategy based on OIG guidance and market trends. The role of billing compliance needs to be increasingly data-driven and cross-functional. It should also include serving as a business partner to other teams including coding, revenue integrity, finance, pharmacy, and clinical, to meet changing and more complex risks. The MDaudit analysis also found that:
- Correctly coding and billing professional and hospital claims can retain 15%-25% of overall revenue.
- Significant revenue opportunities are available for healthcare organizations ensuring proper billing and coding of procedures, drug utilization, and modifiers on professional outpatient claims. Out of 1 million claims with an average of 77% accuracy, 230,000 undercoded claims with the wrong CPT/HCPCS codes ($24 per claim) would result in $5.5 million in additional revenue.
- Errors made in the billing and coding of hospital claims are more costly and offer a significant opportunity for organizations to get diagnoses, DRG, drug units, and procedures correct. For example, out of 100,000 claims with an average 90% accuracy, 10,000 claims with missed or wrong DRG codes ($2,900 per claim) would result in $29 million in additional revenue.
- Compliance teams should have a consistent playbook for auditing over-coded E&M claims, appealing denials to payers, and educating providers on mistakes, as commercial and federal payers are activating external audits to recover erroneous payments.
- Revenue integrity teams can proactively go after the high-dollar claims that are denied and have the biggest impact on their revenue stream. This includes outpatient surgeries, specialty drugs, DMEs and complex diagnoses.
A Technology-based Defense
Based on the Benchmark Report, the greatest risk for healthcare organizations, especially those that are increasingly dependent on federal payers, is to carry a larger burden of proof for timely payments, administrative costs, and defending audits. This is why they need to take a page from payers’ books and look to technology such as cloud, AI, ML (machine learning), and predictive analytics – all of which should catalyze health systems to proactively monitor and rapidly address compliance and revenue risks as they emerge.
In a nutshell, the Annual Benchmark Report reveals the tremendous pressure on healthcare organizations to reduce compliance risk while optimizing revenue flow. Doing so will require flawless optimization for billing compliance, coding, revenue cycle, and revenue integrity capabilities. Yet amidst all the challenges confronting them, the report offers many opportunities for health systems to accelerate digital initiatives and drive sustainable value with analytics, automation, collaboration, and upskilling people.
Download a copy of the MDaudit Annual Benchmark Report.