It is not surprising that there has been an increased focus on preventing denials. The percentage of denied claims has been growing for years and the challenges brought on by the pandemic in 2020 exasperated the problem.
Reducing denials has multiple benefits. Some of them include:
- Cash acceleration
- Reduce days in accounts receivable
- Bad debt reduction
- Decrease of billing compliance issues
- Reduction in staff time spent working denials
To put it simply, reducing the number of denials will have a positive effect on the revenue of an organization.
Reducing denials is not only the responsibility of the business office, it is a team effort that should include revenue cycle, compliance, and clinical stakeholders. It is only possible to make a meaningful impact through collaboration and organizational commitment to improvement. Plus, having the right technology is needed to help an organization identify the problem, educate the source of the problem, and measure the results.
Understanding The Source of Denials
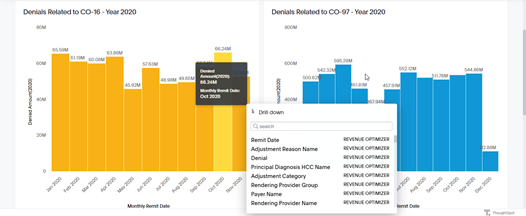
The first step to reduce the number of denials in your healthcare organization is understanding the source of your denials. Many business offices are overwhelmed trying to identify the “real denial” reason. It is like “looking for a needle in a haystack”. That is where the right technology comes into the picture.
A solution like MDaudit’s Revenue Optimizer uses your organization’s remit data to focus on where denials are coming from and drill down to discover the root cause. For example, when looking at the denials experienced, you may discover the most common reason is “The benefit for this service is included in the payment/allowance for another service/procedure that has already been adjudicated.” Then by drilling even further you may discover that the bulk of the denials are attributed to a specific procedure or provider.
By identifying the root cause of denials, your organization can do more than simply correct the claim and resubmit it, your organization can implement educational plans to avoid it happening in the future.
Education and Collaboration
This is the step where having the cooperation of your broader organization is critical. If your business office or revenue integrity department is responsible for denial management, it’s critical that they share the causes of denials with the appropriate stakeholders as those insights are identified.
Distribute the insights among your HIM team and coders so they can learn to avoid the errors in the future. Compare notes with the billing compliance staff to see if they are discovering similar tends in their retrospective audits and work together to identify critical areas to focus audits. Ensure your clinical stakeholders understand the significant financial impact of incorrect coding and documentation and educate them on what changes are needed.
Introducing Prospective Auditing to Your Organization
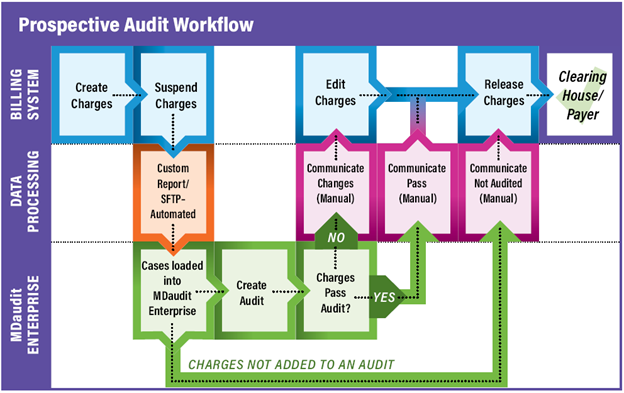
Prospective auditing is simply the process of holding charges for a period of time before submitting the claims, allowing auditors a chance to review a selection of the charges and stop problematic ones from being submitted and subsequently denied. This prospective review of claims works when armed with the right technology, subject matter expertise, and a willingness to collaborate and communicate between departments.
As you can imagine, it would be impossible to audit all claims prior to submission. This is why focusing audits on the procedures, providers, and coders that are most frequently at the source of denials can make a real impact on reducing the total number of denied claims.
Many of our news clients get started by focusing the prospective audits on the highest value claims, then adding in a focus on the most commonly denied claims to make a big impact quickly.
You may be asking yourself “Why do I need to do prospective audits when I have claims editing tools already?” A better question to ask is “Why are my current claims editing tools failing to identify all potential denials?” We find that approximately 30% of the denied claims in the MDaudit community are due to “unspecified” denial reason category. Current claims editing tools perform well on identifying billing-related issues, however clinical protocols, orphan or off-label drug utilization, AWP, and pharmaceutical charges are common gaps. By implementing prospective audits and focusing efforts with the insights you find in your denials, you can prevent those denials commonly missed by claims editing tools.
MDaudit Enterprise Can Help
MDaudit Enterprise is a powerful auditing, integrity, and analytics platform for all your billing compliance and revenue integrity needs. Request a demo to see for yourself how MDaudit enables prospective and retrospective audits and provides insights into your organization’s denied claims.