The devastation of COVID-19 is being felt in every corner of our world. The healthcare industry is at the forefront of the battle, with doctors and nurses fighting the disease on an hourly basis. Data and analytics are playing a key role in helping all of us monitor the progress of the disease, as well as the global healthcare community’s efforts to contain it.
At Hayes we have also been studying the impact of COVID-19 by scanning the data at a high level across our MDaudit Enterprise community. What we are seeing on COVID-19 is just a snapshot of the overall impact, but certainly highlights the scale of the virus.
Since January 1, 2020, our member organizations have performed 150,000+ COVID-19 related services. While many observers are focused on the confirmed cases, we have also viewed the monitored cases, which represent a substantial financial impact and disruption to the healthcare system. According to our data, delivering those services has cost the MDaudit Enterprise community nearly $200+ million. As the crisis continues, the overall financial toll on the healthcare industry continues to rise. The 2-trillion dollar government stimulus package will certainly help as hospitals and providers continue to battle the disease.
Accounting for this influx of cash, and ensuring your organization receives the payments to which it is entitled, however, can quickly become a challenge. New procedure and billing codes – along with changing treatment regulations and reimbursement policies to accommodate the treatment of COVID-19 – are ongoing, and the situation remains fluid. For example:
- Medicare is foregoing a scheduled 2% merit increase to hospitals and providers but is increasing payments on COVID-19 cases by 15%.
- There are new telehealth rules and procedure codes for testing – specifically 99213, 99214 – along with a place of service code to support payment for these services provided to beneficiaries “in any healthcare facilities and in their home.”
- Adding an appropriate modifier can increase payment from $180 to $220 for each engagement, a 22% increase.
While these changes are necessary to meet the challenges of treating COVID-19, the resulting impact to billing and compliance teams promises to last long after the disease is brought under control. To maintain some semblance of financial control today and in the future, revenue cycle and compliance teams must be acting now.
With the amount of money the federal government is pouring into the healthcare system, you can be sure that they will eventually embark on an extensive review process to ensure the legitimacy of all COVID-19 related claims.
Focusing on two main areas now can go a long way toward minimizing problems in the future.
1. Start auditing COVID-19 claims now for compliance
When the virus began to hit, there weren’t specific codes in place to identify COVID-19 cases. Your organization was likely using generic codes around pneumonia, exposure or some kind of virus. Lab tests were also being documented with generic codes and claims for services were being submitted accordingly. As of April 1st, there are now designated diagnoses codes for COVID-19 that must be used to ensure proper reimbursement.
There are already questions being raised about accounting for the actual cases versus those that were reported (1,2). Monitoring cases before and after the new codes were established will be extremely difficult. The government and third-party carriers are not going to accept every claims submission as being legitimate and meeting the new requirements as they pertain to COVID-19.
Once things settle down, there will be a high level of scrutiny around claims for COVID-19 treatments. To address these issues, healthcare organizations should start auditing COVID-19 claims now for proper coding and clinical documentation – for engagements that took place before and after the new codes and regulations were put in place. This auditing can help ensure you are submitting claims correctly to minimize rejections.
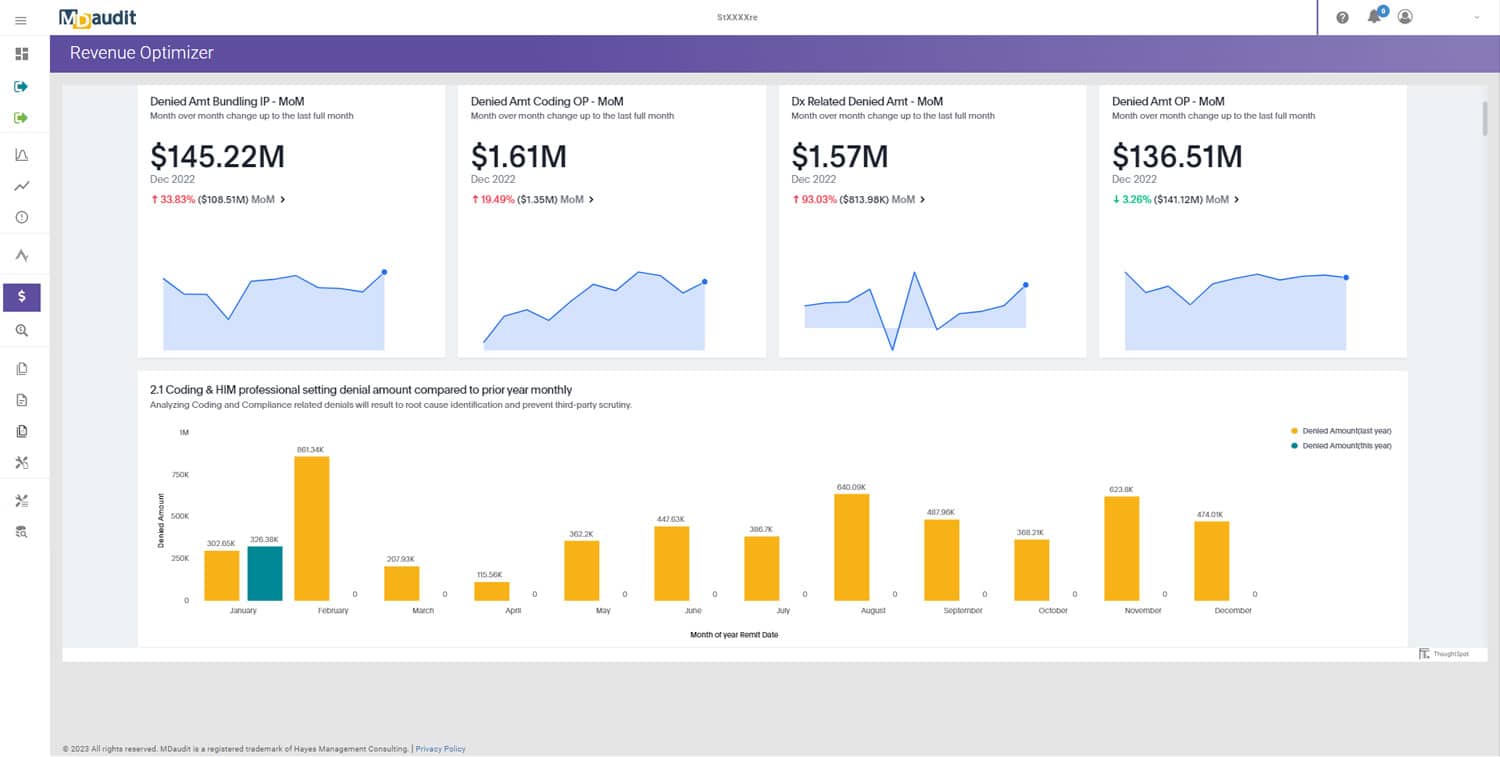
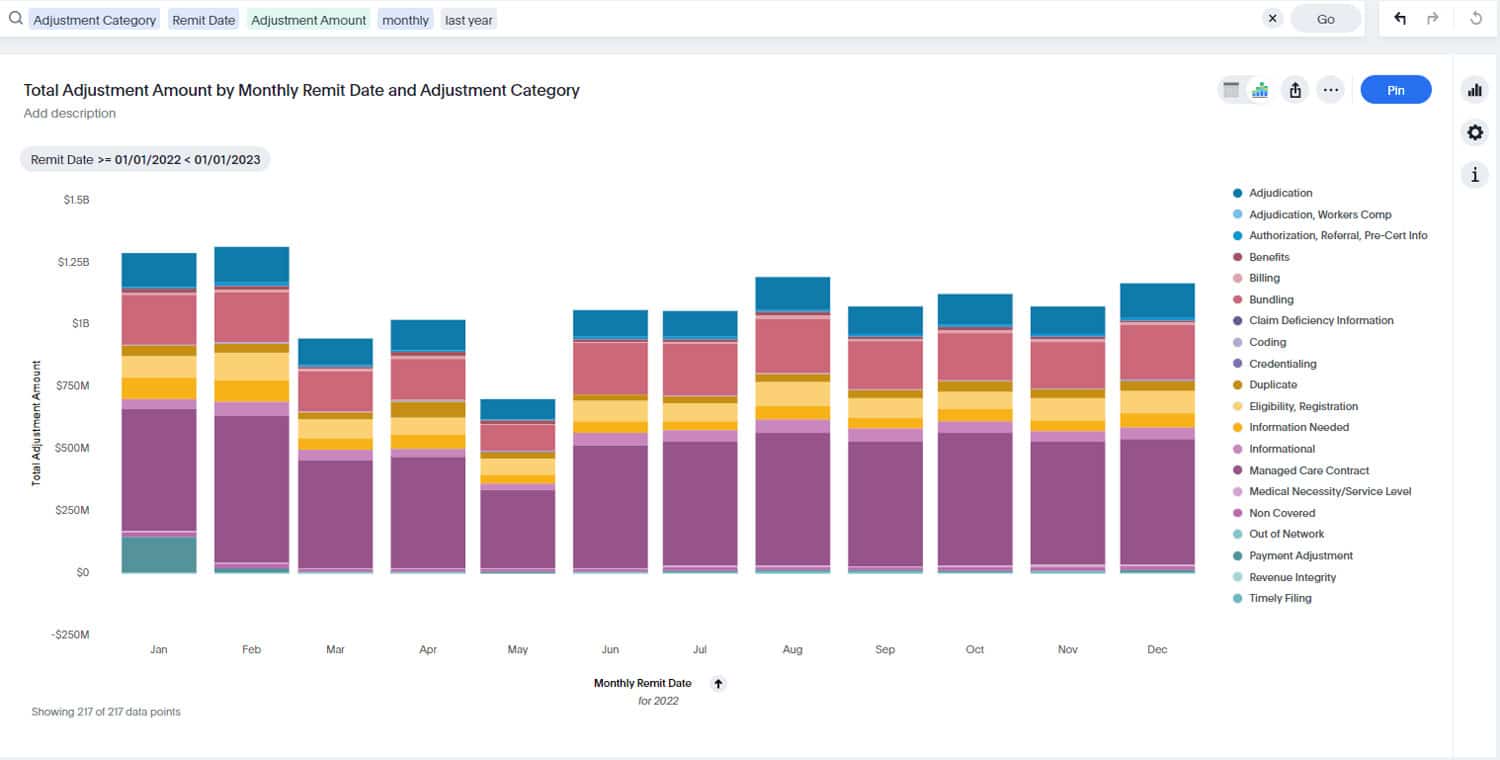
Our MDaudit Enterprise platform can be instrumental in helping you conduct the necessary auditing to ensure proper claims submission. Hayes recognizes the challenges you are facing and is actively monitoring updates and guidelines from the CMS, CDC, and AMA to support the changes. We are releasing updates to MDaudit Enterprise to help you monitor and manage the rapidly evolving regulatory and reimbursement policies being issued in response to the pandemic.
For example, we recently released two new ICD10 codes in the platform to assist in tracking COVID-19 cases, and we will continue to issue updates in response to changing guidelines. Including these codes in our platform enables rapid case searches to monitor and audit COVID-19 services and procedures. In addition, we are adding risk area worksheets for professional billing around virtual check in, online digital E&M, telehealth online assessment, and e-visits. We have also added curated case search for hospital billing, based on the new ICD-10 DX codes, as well as analytics to monitor claims adjudication and denials.
2. Begin monitoring delayed or denied claims for optimal reimbursement
Auditing to ensure proper claims submission is a first step, but it is also critical to start monitoring delayed or denied claims as well. Incorrect or incomplete claims that require adjudication can wreak havoc on your revenue stream.
Because of the urgency and confusion that exists today, there may be a lack of attention on payment delays and denials. To prevent that from happening, set up a mechanism to monitor delayed adjudication so that you can get to the root cause quickly and institute corrective action to ensure that claims are submitted with all the correct codes and documentation.
MDaudit Enterprise is helping you dig deeply into your data to uncover reasons for delayed and denied claims by setting up analytics that encompass different scenarios for you to be able to monitor adjudication issues related to COVID-19 services.
With the amount of money the federal government is pouring into the healthcare system, you can be sure that they will eventually embark on an extensive review process to ensure the legitimacy of all COVID-19 related claims. Get your house in order now to be prepared for the inevitable scrutiny that lies ahead. Preventive preparation is the best defense against having your revenue cycle dramatically disrupted now and in the future.
(1) Coronavirus Case Counts Are Meaningless, FiveThirtyEight, April 4, 2020* https://fivethirtyeight.com/features/coronavirus-case-counts-are-meaningless/
(2) Coronavirus death toll: Americans are almost certainly dying of Covid-19 but being left out of the official count, Washington Post.
https://www.washingtonpost.com/investigations/coronavirus-death-toll-americans-are-almost-certainly-dying-of-covid-19-but-being-left-out-of-the-official-count/2020/04/05/71d67982-747e-11ea-87da-77a8136c1a6d_story.html