The change brought about by healthcare’s greater reliance on technology—especially as it relates to data access and analytics—during the COVID-19 pandemic will likely be permanent, with its greatest impact on care and operational efficiencies, as well as actionable response. As COVID-19 cases continue surging, healthcare organizations’ dependence on guidance and advanced systems to optimally care for patients increases in tandem.
As I discussed in “Proactively Addressing Revenue Integrity in the Era of COVID-19,” published in Compliance Today, prioritizing revenue integrity strategies has also taken center stage as COVID-19 continues to ravage the nation. Analytics are playing a key role in monitoring the virus’s progression and global containment efforts while also laying the groundwork for sound revenue integrity practices within a fluid and evolving crisis.
Because the revenue risks associated with the pandemic will be substantial, compliance and revenue integrity departments must be proactive in preparing for the inevitable scrutiny that lies ahead for COVID-19 related claims to ensure their organizations’ ongoing success and sustainability. Hospitals must capitalize on all appropriate reimbursement opportunities and avoid the revenue cycle bottlenecks that can result from denied or delayed claims. They must also rapidly and proactively identify and address compliance issues to avoid the potential for bottom-line losses during future audits.
This oversight and readiness can’t happen without proper resource allocation and appropriate infrastructures capable of overcoming a fluid regulatory landscape and other challenges. Manual efforts to stay ahead of evolving procedure and billing codes, treatment regulations, and reimbursement policies will leave many healthcare organizations reacting to revenue risks—a retrospective approach that leaves the door open for revenue problems that can quickly spiral out of control. It’s why forward-thinking organizations are getting their revenue integrity house in order now.
A Closer Look at Revenue Shortfalls
Preparations for and response to the pandemic have put providers in the middle of a perfect storm of revenue hits. To free up beds and resources in anticipation of significant demand, the elective procedures that make up a significant portion of income for many hospitals and surgery clinics were halted for greater than a month in most cases. Emergency room visits also dropped substantially amid stay-at-home orders. When combined, these measures are driving long-term revenue losses in the millions for most healthcare organizations.
Reimbursement opportunities have shifted to patient care associated with COVID-19—an area largely untested in terms of payer expectations, claims denials and compliance. There is a lot of money at stake: An internal analysis of the Hayes provider community found that member organizations had performed more than 180,000 COVID-19 related services in the first four months of 2020, exceeding $420 million in overall charges.
Notably, this analysis included both confirmed cases and patients undergoing monitoring for the coronavirus, a distinction that could become important in terms of revenue shortfalls. Foregoing its scheduled 2% merit increase to hospitals and providers, Medicare instead made a strategic decision to increase payments on COVID-19 cases by 20% to address potential revenue losses. Yet, many healthcare organizations may find that this increase falls short of expectations as it only applies to confirmed cases.
For many hospitals, the unfortunate reality is that COVID-19 admissions have not reached scale against financial losses. At the same time, length of stay for pneumonia and sepsis patients has tripled compared to 2019, largely due to COVID-19 monitoring. As a result, reimbursement will not likely cover elective procedure revenue losses. In fact, one study found that 97% of health systems will likely lose an average of $1,200 per case—in some instances as much as $8,000 per case—offset only by the Medicare’s 20% payment increase.
Too, it’s important to bear in mind that cost analysis and contract negotiations for specific DRGs like pneumonia and sepsis were based on 2019 data.
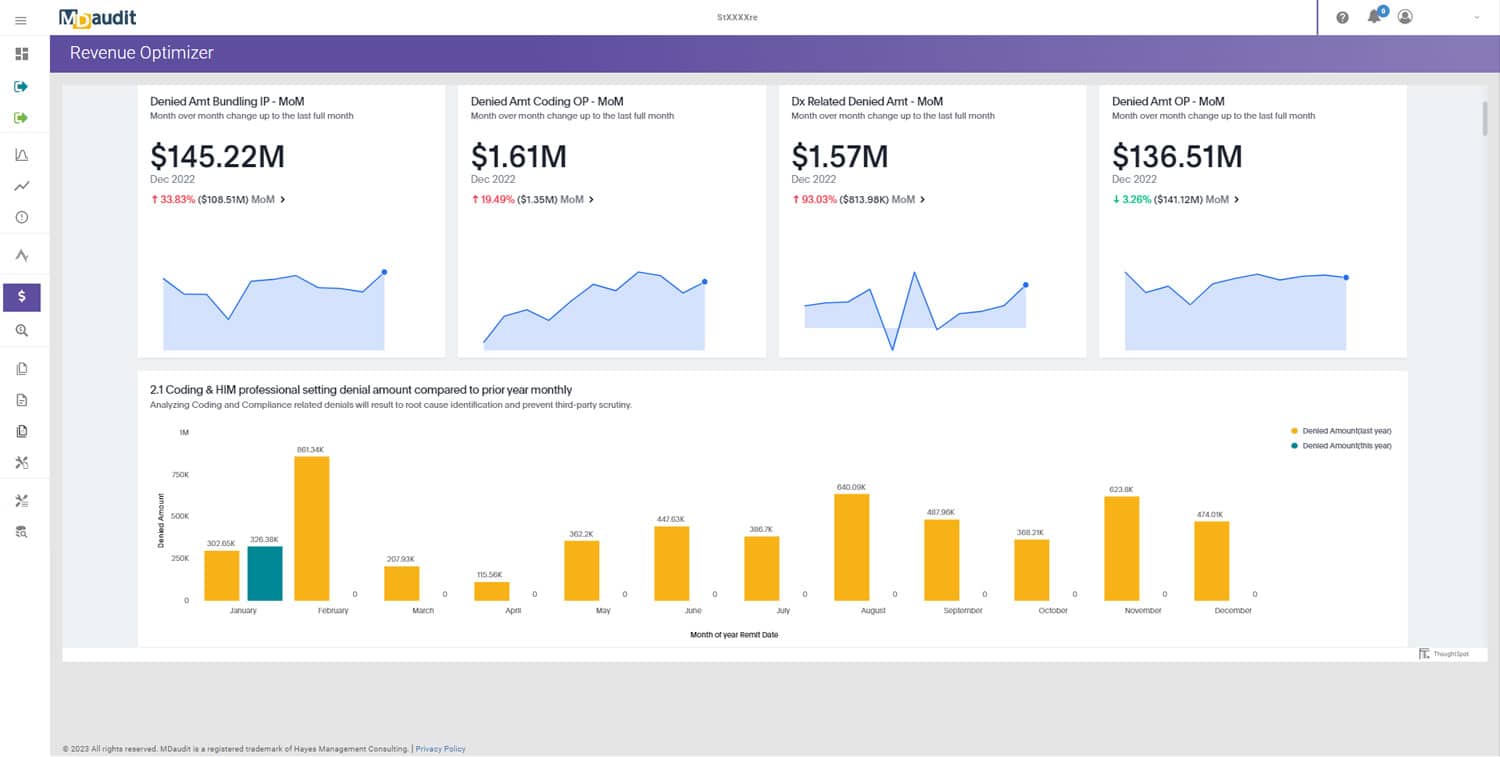
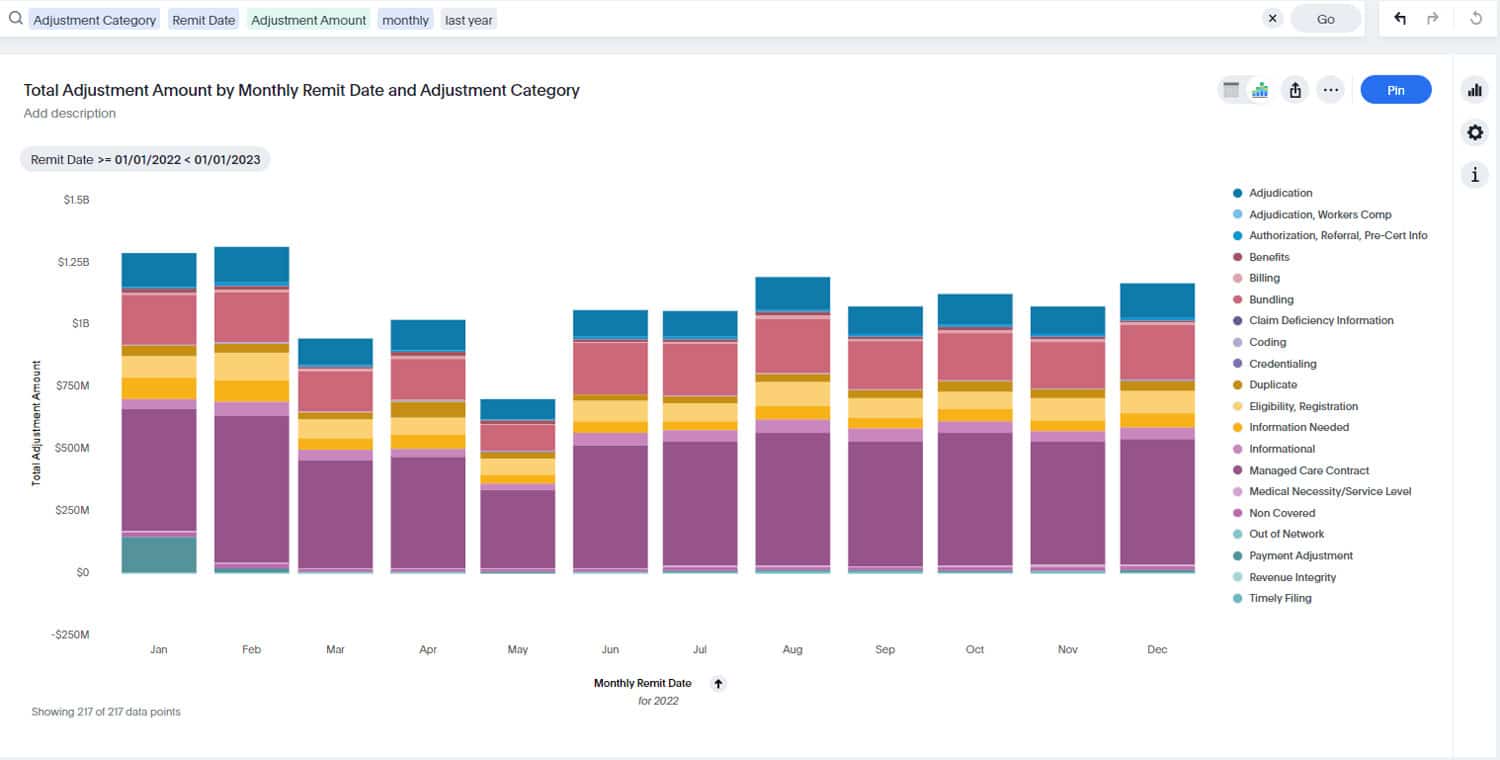
A Bump in Denials
As if revenue shortfalls weren’t enough, healthcare organizations can also expect an increase in denials. History demonstrates that any time new rules and procedure codes are enacted, issues surface as the industry learns how to interpret new guidance. With COVID-19 came a plethora of changes, including new telehealth rules, modifiers, procedure codes for testing, ICD10 codes and a place-of-service code to support payment for services provided to beneficiaries in any healthcare facilities and in their home.
While these changes are necessary, their impact on billing and compliance teams is creating headaches. For example, in the very early stages of the pandemic, there were no specific codes to identify COVID-19 cases, so coding departments likely used generic codes related to pneumonia or exposure to a virus. Generic codes and claims were also like used to document lab tests, making it difficult to account for actual cases. And while designated diagnoses codes for COVID-19 were introduced in April, monitoring cases before and after the new codes were established will be extremely difficult for providers.
Amid all this chaos, one thing is certain for healthcare organizations: Government and private payers are not going to accept every claim submission as a legitimate COVID-19 case that meets current requirements.
Read part two of this two-part series which delves into revenue integrity readiness strategies to mitigate the potential that these impacts will do lasting damage.
Interested in learning more about revenue integrity? Click here to download our whitepaper “An Unexpected Marriage: Tying the Knot Between Compliance and Revenue Cycle to Ensure Revenue Integrity”.