The rate that medical claims are being denied is steadily increasing and it is trend that will cost your organization millions, if not billions over the next few years. MDaudit Enterprise customers saw an 8% average increase in the number of denials from 2019-2020, and so far, 2021 doesn’t look any better.
Along with delaying the payments you are owed, the increase is also causing bottlenecks in denial departments. Many denial teams are struggling to keep up with the volume for a variety of reasons.
- New and changed coding and billing rules and guidelines
- Overwhelmed staff and the lack of bandwidth
- Delays in getting data for reporting and analysis due to IT’s workload
- Pressure from the complexities COVID-19 has presented
This is a problem that can’t be corrected without taking a step back and reevaluating the efforts of your team and their approach to working denials. Are they working as efficiently as they can? How do you know?
Trying to understand and quantify how well your denial department is doing may seem easy at first glance, but the numbers you look at today probably don’t tell the right story. For example, if you look at how many claims were touched, can you tell if the proper research was done or if the claim was even corrected before resubmission? Does the department simply work to correct the claim and resubmit it or do they dig into the root cause of the denial and work to educate physicians and coders to prevent it from happening again?
A better approach to managing your denial department is to identify the right metrics that measure not just quantity, but also quality of work, and then ensure those are the metrics you use to measure each team member against. Start the process by working with your team to set goals for each person. Make them SMART goals that are specific, measurable, attainable, relevant and timely. Having clear goals for each person, not just the organization, will allow your team members to understand what is expected and give them something to strive for.
Some examples of what you should measure are:
- Year-over-year or month-over-month denial trends. Your team should be communicating what they find to education others to avoid future denials – and as a result, dropping the number of and value of denials.
- Timely adjudication, especially of the highest value claims.
- Reduction in the number of specific types of denials that should be avoidable, such as incorrect usage of Modifier 25.
- Workload by team’s work assignment to ensure even distribution and avoid bottlenecks when possible.
- Denial reasons by department responsible for the denial to help establish collaboration and develop future mitigation strategies.
By taking a data driven approach to understanding where denials are originating from and the reasons, the denial team can become more effective at working the denials quickly and mitigating future denials.
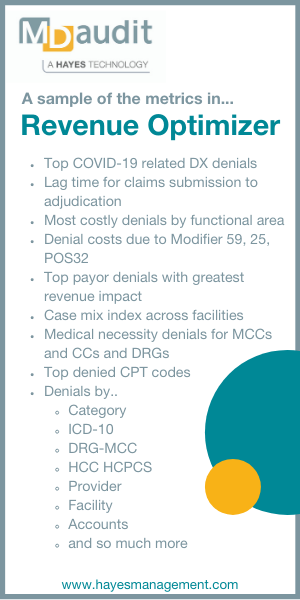
A common argument against measuring these types of metrics is that the numbers can’t be easily calculated, or they can’t be calculated without hours or days of manual data analysis and extensive spreadsheets. A solution such as MDaudit Enterprise’s Revenue Optimize can help. This Augmented Intelligence solution allows healthcare organizations to monitor denial trends, detect anomalies that should be investigated, and drill down across 35+ variables using natural language search. The drill-down capabilities are invaluable for truly understanding the cause of denial by allowing healthcare organizations to look at denials by provider, procedure, date, payer and so much more.
To learn more about setting individual goals, key metrics to track and how MDaudit Enterprise can help, view our on-demand webinar “How to Improve Your Denial Department’s Productivity and Effectiveness”.