Revenue cycle management (RCM) challenges appear here to stay, and the question is not how to get rid of them but how to succeed despite them.
Recent reports show that operating margins are continuing to improve following COVID-19. Despite these tailwinds, RCM professionals continue to face the same restraints as in previous years around labor shortages, timely payer reimbursements, cybersecurity issues, and financial instabilities.
Against this backdrop, RCM transformation is one of the most strategic initiatives for health systems to prioritize. Regulatory headwinds and external pressures are not going away anytime soon, and even with supportive tailwinds, revenue cycle leaders are looking for solutions to build a sustainable financial future.
RCM leaders must take a progressive, data-driven, people-led, and technology-enabled approach. This approach encompasses a holistic workflow focusing on continuous risk monitoring and actionable data insights.
The Evolving Landscape of Revenue Cycle Management
Regulatory changes, reimbursement shifts, and increasing scrutiny from The Office of Inspector General (OIG) all indicate the need for improved RCM processes. Organizations must be able to understand the evolving trends around payer behavior while allocating resources to drive sustainable financial outcomes. This may have sounded like a pipedream several years ago, but such actions are possible with the right technology and a data-driven approach.
Today’s healthcare organizations face various challenges that can hinder their ability to maintain financial stability and compliance. Coding complexities arise from frequent regulatory updates, evolving payer requirements, and the need for precise documentation to avoid denied claims or underpayments. This intricacy often leads to errors, creating vulnerabilities during audits.
At the same time, audit risks have escalated as government and private payers intensify scrutiny, particularly in areas like billing compliance and medical necessity. According to data from the MDaudit community, external payer audits increased 2.2x, and at-risk dollars increased 5x in 2024 vs. 2023 across commercial and government payers.
Revenue leakage, which can occur through inefficiencies such as missed billing opportunities, inaccurate coding, or unaddressed denials, compounds these issues. These challenges demand a proactive, integrated approach to mitigate risks, optimize reimbursements, and safeguard organizational revenue.
The Data-Driven Advantage
Why Data is Crucial for RCM Success
Data is the backbone of modern revenue cycle management, empowering healthcare organizations to make informed decisions directly impacting financial performance. Real-time analytics and insights enable organizations to monitor billing patterns, identify anomalies, and address potential compliance risks before they escalate into revenue loss. This level of immediacy enhances decision-making and allows for rapid course correction.
In addition to real-time data, historical data provides invaluable context. Organizations can predict future challenges by analyzing past trends, such as denials or audit vulnerabilities, and implementing preventive strategies. Leveraging both real-time and historical data ensures a comprehensive, proactive approach to maintaining financial health and compliance.
2. Building a Culture of Data Integrity
A successful data-driven strategy hinges on the accuracy and reliability of the data itself. Ensuring accurate and comprehensive data collection starts with standardized processes for documentation and billing, supported by robust training for staff across departments. Technology plays a key role here, with advanced platforms capable of flagging inconsistencies and automating error-prone tasks.
However, technology alone isn’t enough. Compliance and risk assessment must be embedded in the organization’s data governance strategy. This involves regular audits, clear accountability structures, and adherence to industry best practices for data security and integrity. Organizations that foster a culture of data accuracy set the foundation for actionable insights and informed decision-making.
3. Actionable Insights for Improved Outcomes
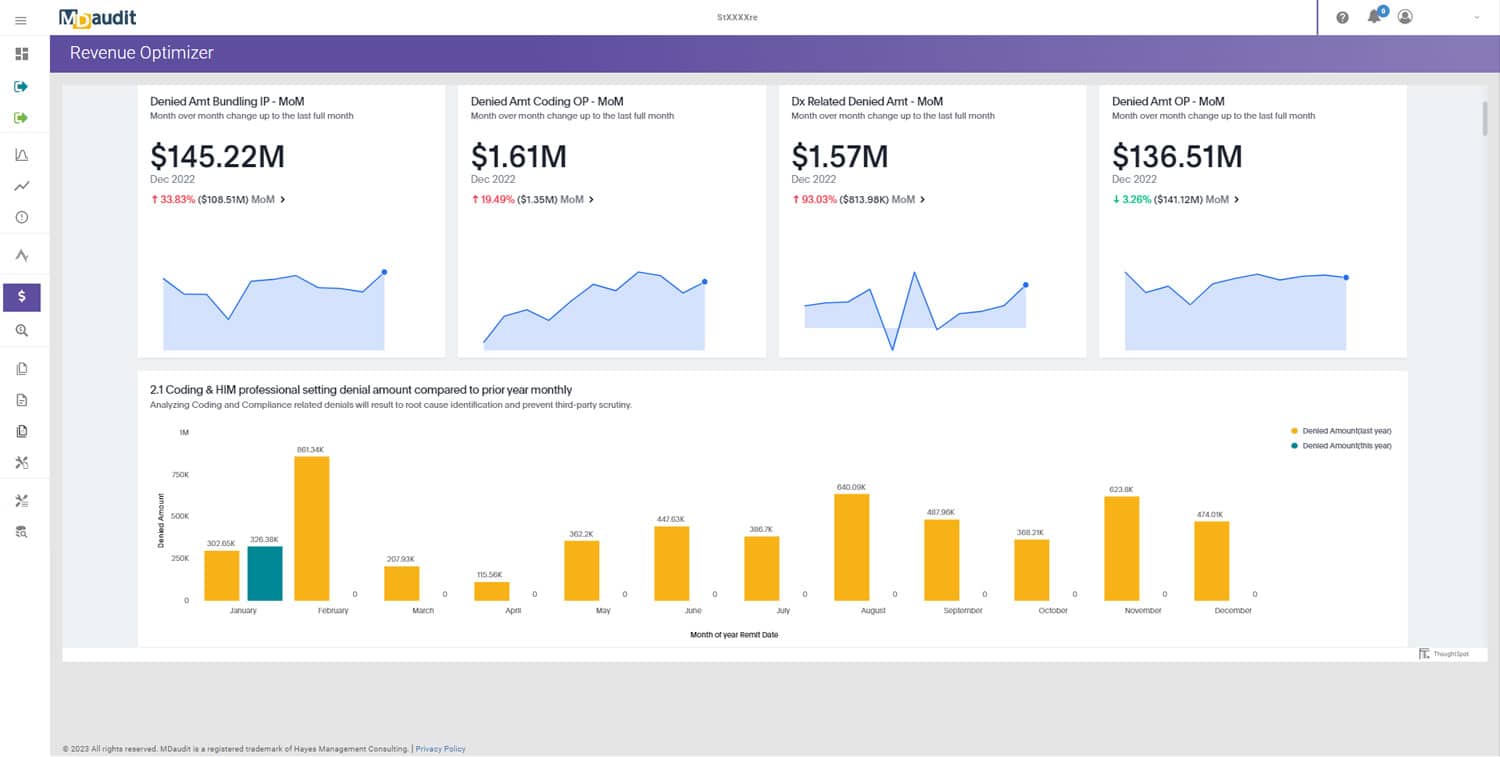
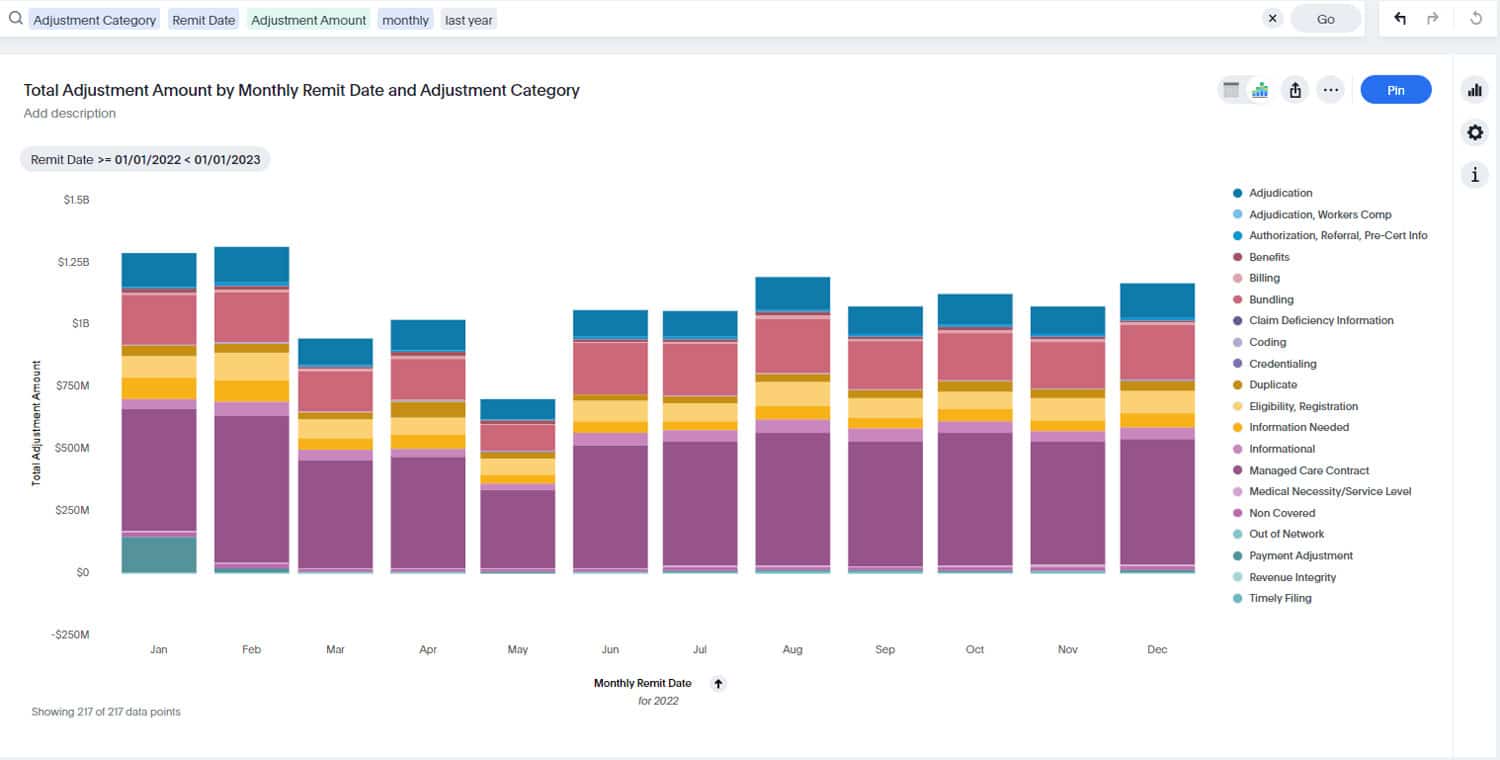
A data-driven approach aims to translate raw data into actionable insights that drive meaningful outcomes. For example, denial management analytics can identify recurring reasons for claim rejections, prompting corrective actions, such as providing physician education or updating coding protocols. Predictive analytics can anticipate areas of revenue leakage, allowing proactive interventions that optimize reimbursements.
Organizations must track critical metrics and key performance indicators (KPIs) to achieve these outcomes, such as denial rates, days in accounts receivable (A/R), clean claim rates, and audit findings. These indicators provide a clear snapshot of performance, enabling teams to align their efforts with organizational goals and continually refine processes for better outcomes.
Empowering People to Lead Change
Cross-Functional Collaboration
The complexity of RCM requires seamless collaboration between coding, billing, revenue integrity, and clinical teams to achieve optimal outcomes. Each department plays a critical role; miscommunication or siloed operations will result in errors, delays, or lost revenue. Bridging these gaps involves fostering an environment of mutual understanding and shared objectives. For example, clinicians can benefit from education on how accurate documentation supports coding and billing, while coders and billers can gain insights into the clinical context of their work. Regular interdisciplinary meetings, shared performance dashboards, and clear communication channels ensure that all teams are aligned and working cohesively toward organizational goals.
Fostering a Culture of Continuous Improvement
A people-led RCM strategy thrives when teams are motivated by a shared commitment to excellence. Engaging staff with transparent performance metrics and goals is a crucial step. By providing visibility into KPIs, organizations empower employees to understand how their efforts impact overall performance. These metrics should be paired with ongoing training and feedback to help staff continuously enhance their skills. Moreover, fostering a culture of innovation is vital. Rewarding adaptability and creative problem-solving boosts morale and drives process improvements. Organizations that recognize and celebrate staff contributions, whether through professional development opportunities, incentives, or recognition programs, create a motivated and resilient workforce who can navigate the challenges of RCM.
Change Management
Change is difficult and does not happen overnight. Remember the importance of organizational buy-in; when everyone is rowing in the same direction, this RCM approach can deliver healthier bottom lines.
Technology as the Catalyst for Transformation
1. The Power of Continuous Risk-Based Monitoring
Technology has revolutionized how healthcare organizations approach RCM, particularly in addressing audit risks and revenue leakage. Continuous risk-based monitoring enables organizations to proactively identify and mitigate compliance vulnerabilities by analyzing real-time claims data.
This reduces the likelihood of costly audits and ensures that claims are processed accurately. Moreover, automation in billing compliance audits streamlines repetitive tasks, such as flagging discrepancies and verifying documentation, freeing up staff to focus on higher-value activities like education and process improvement. By embedding these technologies into RCM workflows, organizations enhance both accuracy and efficiency.
2. Integrating Advanced Technology into the RCM Workflow
Modern RCM platforms are equipped with advanced features that harness the power of artificial intelligence (AI) and analytics to optimize operations. These platforms can analyze large datasets to identify patterns, predict denials, and recommend corrective actions, empowering teams with actionable insights.
Furthermore, these technologies streamline coding, auditing, and reporting processes, ensuring greater accuracy and compliance with less manual effort. For example, automated coding solutions can reduce errors, while predictive analytics can help organizations allocate resources effectively. By seamlessly integrating these technologies into existing workflows, healthcare organizations can improve performance and reduce operational friction.
3. Scaling Technology for Long-term Success
To remain competitive and resilient, healthcare organizations must prioritize scalable and interoperable solutions that can evolve alongside industry demands. Scalable platforms allow organizations to accommodate growth, adapt to new regulations, and incorporate additional functionalities as needed.
Interoperability ensures that these systems can integrate with existing technologies, creating a unified and efficient RCM ecosystem. Beyond operational benefits, the return on investment (ROI) of adopting technology-enabled solutions is significant, including improved cash flow, reduced denials, and better staff productivity. By investing in future-ready technologies, organizations set themselves up for sustained success in an ever-changing healthcare environment.
Success in Action
A large multispecialty practice with more than 3,500 physicians and encompassing more than 250 specialties and services faces the challenge of massive audit volume that clashes with manual systems. “There was no way for us to be able to share the impact- or even know what the impact was because we could never get through all the audits in a year,” shares the Associate Director for Audit Compliance Education.
With a continuous risk monitoring platform, this practice reduced audit preparation time from one week to one hour. It also realized $14 million in claim charges, 16,590 cases audited, and $1.9 million in additional revenue.
The Blueprint for Implementing a Data-Driven, People-Led, and Technology-Enabled Strategy
1. Assessment and Gap Analysis
A successful transformation in RCM begins with a thorough assessment and gap analysis to pinpoint areas that need improvement. This involves evaluating the current RCM process to identify pain points such as recurring claim denials, workflow inefficiencies, or underutilized technologies. Simultaneously, organizations should uncover opportunities to enhance performance, such as adopting an advanced platform, improving staff training, or refining data collection practices. This comprehensive analysis is the foundation for a strategic plan tailored to the organization’s needs.
2. Building the Foundation
With insights from the gap analysis, the next step is to align data, people, and technology goals with overarching organizational objectives. This alignment ensures that every component of the RCM strategy supports financial, operational, and compliance targets. For example, data analytics should prioritize actionable insights that drive decision-making, while staff training programs should empower teams to leverage technology effectively. Establishing this foundation requires clear communication of goals, cross-departmental collaboration, and leadership buy-in to create a unified vision for transformation.
3. Implementation Roadmap
Transitioning to a data-driven, people-led, and technology-enabled RCM model requires a detailed step-by-step roadmap. This roadmap should outline the integration of data analytics, the rollout of staff training programs, and the deployment of advanced technology solutions. It’s crucial to prioritize scalable solutions that can adapt to future needs and to implement changes in manageable phases to minimize disruption. Pilot programs can test new approaches before scaling them across the organization. Regular milestones and checkpoints ensure progress is tracked and adjustments are made as necessary. The right platform will be accompanied by robust training and implementation by the vendor alongside ongoing training to support your organization.
4. Measuring and Refining the Approach
To sustain success, organizations must establish a feedback loop for continuous improvement. This involves regularly measuring KPIs to assess the effectiveness of the implemented strategies. Feedback from staff and stakeholders is equally important to identify challenges and opportunities for refinement. By fostering an environment of continuous learning and adaptation, healthcare organizations can ensure their RCM approach remains effective and resilient in the face of evolving industry demands.
MDaudit’s mission is to help you reap all the benefits of a data-driven, people-led, and technology-enabled RCM approach. By adopting this strategy, healthcare systems can build a sustainable financial future for those they serve.