Revenue integrity is a crucial pillar in the healthcare industry, ensuring organizations optimize their financial performance while maintaining compliance with regulatory standards. In an era of increasing scrutiny and complex reimbursement landscapes, a robust revenue integrity strategy is more essential than ever.
A Holistic Revenue Integrity Ecosystem
A holistic revenue integrity ecosystem goes beyond the traditional scope of billing and coding. It encompasses a wide range of factors including data analytics, continuous risk monitoring, cross-departmental collaboration, and proactive compliance measures. This ecosystem ensures that every aspect of the revenue cycle is interconnected and aligned with the organization’s broader financial and operational goals.
This holistic ecosystem is fueled by integrating advanced technologies and fostering a culture of continuous improvement. At its core, revenue integrity aligns an organization’s processes, people, and technology to ensure accurate and compliant revenue generation. This involves the seamless coordination between clinical documentation, coding, billing, and reimbursement processes to minimize errors, reduce compliance risks, and maximize revenue capture.
Holistic revenue integrity programs not only safeguard against financial losses but also promote sustainable growth and operational efficiency. This whitepaper explores the concept of creating a holistic revenue integrity ecosystem, offering insights and strategies for healthcare leaders to build and sustain a system that supports financial and organizational excellence.
Defining Revenue Integrity
Revenue integrity in healthcare refers to ensuring that all clinical services are accurately documented, properly coded, and correctly billed to optimize revenue while maintaining compliance with regulatory standards. It encompasses a range of activities, including:
- Accurate coding of medical procedures and diagnoses
- Timely and precise billing for services rendered
- Continuous monitoring and auditing of billing practices
- Ensuring compliance with federal and state regulations
Revenue Integrity Values:
Financial Stability: Proper revenue management ensures that healthcare providers receive full reimbursement for their services. This financial stability allows organizations to invest in better patient care and advanced medical technologies.
Regulatory Compliance: With the healthcare industry heavily regulated, maintaining compliance is essential. Revenue integrity helps avoid legal issues and potential fines associated with improper billing and coding practices.
Patient Trust: Accurate billing practices foster trust between patients and healthcare providers. Patients who see transparent and fair billing are more likely to trust and continue their care with the provider.
Operational Efficiency: Streamlining revenue cycle processes reduces administrative burdens and enhances overall operational efficiency, allowing healthcare professionals to focus more on patient care.
Revenue Integrity Pillars: Delivering a Healthy Bottom-Line
Many denials originate at the front and middle of the revenue cycle and are triggered by billing, coding, and clinical issues that impact downstream. When anomalies and abnormal events in these areas are proactively and continuously monitored in the mid-revenue cycle and fixed, compliance and revenue outcomes don’t have to compete as conflicting interests. Instead, they can become more strategic and sustainable versus transactional and temporal. This is key to ensuring the delivery of a healthy bottom line.
Revenue integrity pillars help providers improve revenue and ensure compliance with regulations and contracts. Some pillars include:
Compliance and Risk Monitoring: Regular audits and risk assessments help identify and rectify any discrepancies in billing practices, ensuring adherence to regulations. Continuous risk monitoring can also detect anomalies, determine root causes, and compare organizational risk with peer organizations.
Proper Coding: Utilizing correct medical codes for procedures and diagnoses is crucial for receiving appropriate reimbursement. This involves continuous education and training for coding professionals. Along with collaborative communication along the revenue cycle.
Charge Capture: Ensures that all clinical documentation accurately reflects the care provided and billed.
Claims Management: Submitting timely and correct claims helps maintain a steady cash flow and reduces the risk of claim denials. Managing denials and appeals efficiently also limits revenue leakage.
Denial Management: Technological advancements with artificial intelligence (AI) and analytics can now close the gap that traditional claim scrubbers leave behind. With denial prediction, professionals can use data insights to address the charges that drive 80% of denial dollars.
Challenges Maintaining Healthcare Revenue Integrity
Maintaining revenue integrity in healthcare is becoming increasingly complex due to a dynamic regulatory environment, evolving reimbursement models, and the need for advanced technological integration. Here are the top three challenges healthcare organizations face today in upholding revenue integrity:
- Regulatory Compliance and Audits
The regulatory landscape in healthcare is continually shifting, with new laws, regulations, and guidelines being introduced at both federal and state levels. Compliance with these regulations is a significant challenge, as healthcare organizations must stay current with changes while ensuring that all processes are aligned with the latest standards. The Office of Inspector General (OIG) and other auditing bodies are intensifying scrutiny, increasing the risk of audits and potential financial penalties. Organizations must implement comprehensive compliance programs and conduct regular internal audits to avoid breaches that could compromise revenue integrity.
2024 OIG Work Items Impacting Revenue Integrity.
- Evolving Reimbursement Models
The shift from fee-for-service to value-based care models has introduced new complexities in revenue management. Value-based reimbursement ties payments to patient outcomes, requiring healthcare organizations to adapt their revenue cycle processes to reflect this focus on quality and efficiency. This transition involves rethinking traditional billing and coding practices, integrating new performance metrics, and managing the risks associated with fluctuating reimbursements. The challenge lies in balancing the need for accurate revenue capture with the demand for improved patient care outcomes, all while navigating a landscape where reimbursement models are in constant flux.
- Technological Integration and Data Management
As healthcare organizations adopt more advanced technologies, the integration of these systems poses a significant challenge to maintaining revenue integrity. The sheer volume of data generated by electronic health records (EHRs), billing systems, and other healthcare technologies can lead to discrepancies and errors if not managed effectively. Ensuring that data is accurate, consistent, and securely shared across platforms is critical to preventing revenue leakage.
Additionally, the adoption of AI and machine learning tools, while promising, requires careful implementation and monitoring to ensure they enhance rather than hinder revenue integrity efforts. Organizations must invest in robust data governance frameworks and continuous staff training to fully leverage technological advancements without compromising revenue integrity.
These challenges underscore the importance of a proactive, well-coordinated approach to revenue integrity, where compliance, reimbursement, and technology are all aligned to support the financial and operational health of healthcare organizations.
The Need for An End-To-End Approach
Given the complexities and challenges outlined above, maintaining revenue integrity in healthcare requires more than just addressing individual issues as they arise. A fragmented or reactive approach is no longer sufficient in the face of regulatory pressures, evolving reimbursement models, and the demands of technological integration. Instead, a holistic, end-to-end strategy is essential to overcoming these challenges and ensuring long-term financial stability and compliance.
Implementing A Holistic Revenue Integrity Strategy
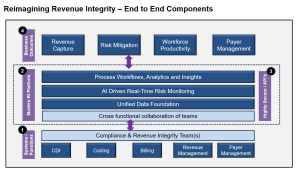
A successful, holistic revenue integrity strategy relies on well-structured systems and functions, with dedicated teams playing key roles in ensuring accurate, compliant, and efficient revenue management. At the heart of these efforts are the clinical documentation integrity (CDI), coding, billing, compliance, revenue management, and payer management teams whose roles are crucial to safeguarding the financial and operational health of healthcare organizations. Understanding their responsibilities and how they work together is essential for building a robust revenue integrity framework.
In healthcare revenue cycle management, various teams play critical roles to ensure accurate and compliant revenue capture.
- The clinical documentation integrity (CDI) team ensures that medical records accurately reflect the patient’s diagnoses and treatment, serving as the foundation for proper coding and billing.
- The coding team translates clinical documentation into standardized codes used for billing, ensuring that all procedures and diagnoses are accurately represented.
- The billing team submits claims to payers based on the coded services and manages the payment process, including handling denied claims and pursuing outstanding balances.
- The compliance team monitors adherence to regulatory guidelines, conducting audits and risk assessments to ensure the organization meets all legal and payer requirements.
- The revenue management team oversees the entire revenue cycle, ensuring that all processes—from patient registration to final payment—are optimized for accuracy and efficiency.
- Finally, the payer management team focuses on negotiating and managing relationships with payers, ensuring that contracts are honored, payments are timely, and disputes are resolved efficiently.
Together, these teams collaborate to create a seamless and efficient revenue cycle that maximizes revenue capture while maintaining compliance and operational excellence.
Cross-functional Collaboration Between Healthcare Teams
While each healthcare team along the revenue cycle continuum has a distinct role, their collaboration is essential for maintaining a strong revenue integrity system. These teams must work in tandem to ensure that compliance efforts do not hinder revenue capture and that financial strategies do not compromise regulatory adherence. This collaboration often involves regular communication, joint training sessions, and coordinated audits that address both compliance and revenue concerns.
The effectiveness of a revenue integrity system depends on the expertise and collaboration of all the teams. By clearly defining their roles and fostering a cooperative approach, healthcare organizations can build a resilient framework that supports accurate, compliant, and efficient revenue management.
This partnership can be taken to the next level with a sophisticated platform outfitted with data analytics, artificial intelligence, and workflows that keep all members of compliance and revenue integrity in the loop.
Defining a Best In-class, Modern Revenue Integrity Platform: Your Solution for Successful Collaboration
A modern revenue integrity platform unites teams and stakeholders across the revenue cycle continuum with the data and analytics necessary to fuel holistic, actional steps related to successful business outcomes.
A Unified Data Foundation
Data is the backbone of effective revenue integrity management. A unified data foundation is essential for ensuring that all teams and stakeholders have access to accurate, consistent, and up-to-date information. By establishing a unified data foundation, healthcare organizations gain necessary insight into the challenges and strategies involved in integrating data across systems, and the significant benefits of creating a single source of truth within healthcare organizations.
The Importance of a Unified Data Foundation
A unified data foundation is critical for maintaining the integrity, accuracy, and efficiency of the revenue cycle. In healthcare, data is generated from a variety of sources, including electronic health records (EHRs), billing systems, patient management platforms, and compliance tools. Without a unified approach, data can become fragmented, leading to inconsistencies, errors, and gaps that compromise revenue capture and compliance.
A unified data foundation ensures that data is standardized and consistently shared across all systems and departments. This enables healthcare organizations to streamline processes, reduce redundancy, and improve decision-making. By ensuring that all stakeholders have access to the same, accurate data, organizations can more effectively manage the complexities of billing, coding, and reimbursement, while also maintaining compliance with regulatory requirements.
Integrating Data Across Systems
Integrating data across disparate systems is a significant challenge in healthcare, but it is essential for creating a unified data foundation. Different departments within a healthcare organization often use various software platforms, each designed to meet specific needs. This can result in silos of information, where data is not easily accessible or shared across the organization.
Effective data integration requires the use of interoperable technologies that can communicate and exchange information seamlessly. This may involve implementing middleware solutions that connect different systems, enabling real-time data exchange and synchronization. Additionally, organizations must establish data governance protocols to ensure that data is accurately mapped, cleaned, and validated during the integration process.
Integrating data across systems facilitates better coordination between departments and supports more comprehensive analytics. When data from clinical, financial, and operational systems is integrated, healthcare organizations can gain deeper insights into their performance, identify trends, and uncover opportunities for improvement.
The Benefits of a Single Source of Truth: A Modern Revenue Integrity Platform
Establishing a single source of truth—a central, authoritative repository where all data is stored and managed—is one of the most significant advantages of a unified data foundation. A single source of truth ensures that all data is consistent, accurate, and accessible to authorized users across the organization. This eliminates the discrepancies and confusion that can arise from using multiple, conflicting data sources.
The benefits of a single source of truth are manifold. First, it enhances the accuracy and reliability of reporting, enabling healthcare leaders to make informed decisions based on comprehensive and trustworthy data. This is particularly important in areas such as revenue integrity, where decisions must be made quickly and accurately to avoid financial losses and compliance issues.
Second, a single source of truth improves operational efficiency by reducing the time and effort required to reconcile data from different sources. Staff can spend less time searching for and validating information, and more time focusing on core tasks such as patient care, billing, and compliance monitoring.
Finally, a single source of truth supports better patient outcomes by ensuring that all healthcare providers have access to the same accurate and up-to-date information. This promotes continuity of care, reduces the risk of errors, and enhances the overall patient experience.
A unified data foundation is the cornerstone of holistic revenue integrity management in healthcare.
AI-Driven Real-Time Risk Monitoring
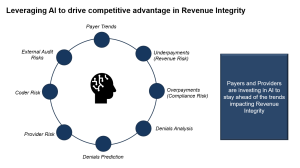
Introduction to AI in Revenue Integrity
Artificial intelligence (AI) is transforming revenue integrity by automating complex processes, enhancing accuracy, and providing deep insights into data. A modern revenue integrity platform should be able to deliver AI-driven tools that can quickly analyze vast amounts of clinical, financial, and operational data, flagging potential risks and uncovering opportunities for revenue optimization.
As regulatory demands and payer complexities grow, AI empowers revenue integrity teams to streamline their workflows, reduce human error, and improve decision-making. AI’s ability to learn from patterns enables continuous improvement in compliance, coding accuracy, and revenue capture, making it a critical asset for healthcare organizations.
Real-time Risk Monitoring Capabilities
AI enhances real-time risk monitoring by providing immediate insights into potential compliance issues, coding inaccuracies, and revenue leakage. By continuously scanning data from billing systems, EHRs, and claims remittance data, AI can identify discrepancies or anomalies that signal potential risk areas. This real-time capability allows healthcare organizations to take proactive action, preventing revenue losses or regulatory breaches before they occur. Automated alerts and predictive analytics ensure that risks are addressed swiftly, improving the organization’s ability to remain compliant while optimizing revenue streams.
Examples of AI Applications in Risk Management
AI applications in risk management are already yielding significant benefits in healthcare. For example, AI can automate the review of claims for compliance with payer guidelines, reducing the risk of denials. Machine learning algorithms can analyze historical data to predict future risks, helping organizations anticipate and address coding or billing issues before they impact revenue. Additionally, AI-powered tools can cross-reference clinical documentation with billing codes to ensure accurate claims submissions, thereby reducing the likelihood of audits and regulatory penalties. These AI applications not only streamline risk management processes but also enhance the overall accuracy and efficiency of revenue integrity efforts.
Process Workflows, Analytics, and Insights
Designing Efficient Process Workflows
Efficient process workflows are essential for managing the complex and interconnected functions of revenue integrity. By designing workflows that are streamlined, automated, and adaptable, healthcare organizations can reduce manual bottlenecks and optimize resource use. AI and machine learning can be integrated into these workflows to assist with tasks such as coding, documentation reviews, and claims submission, ensuring that processes are not only efficient but also continuously improving. Workflow automation reduces the need for manual intervention, allowing staff to focus on higher-value tasks and improving overall productivity.
Leveraging Analytics for Insights
Analytics play a critical role in uncovering trends, identifying inefficiencies, and driving improvements within revenue integrity. By leveraging advanced analytics tools, healthcare organizations can gain actionable insights from their data, such as identifying patterns in denied claims, pinpointing compliance risks, or highlighting revenue opportunities. Predictive analytics, powered by AI, can help organizations forecast potential issues before they arise, allowing for timely interventions. With these insights, healthcare leaders can make informed decisions that optimize revenue, reduce risk, and improve operational efficiency across the organization.
Case study
- A Faith-based, Nonprofit Customer faces the challenges of increased Medicare RAC audit scrutiny that threatens potentially devastating financial risks. With the use of MDaudit’s Denials Predictor, the customer was able to identify denials risks and their root causes- even before payer adjudication- to decrease denials, shorten payment lag time, and increase cash flow.
“With Denials Predictor, I have a simple solution that will stop claims from going out the door without the appropriate designation. It’s insanely powerful. The technology is fantastic.” – Director of Revenue Cycle Compliance
Business Outcomes
A holistic revenue integrity strategy extends beyond regulatory compliance; it drives measurable business outcomes that impact every facet of a healthcare organization’s financial health and operational efficiency. Healthy business outcomes can be measured by the following key performance indicators (KPIs).
Revenue Capture
Maximizing revenue capture is a fundamental goal of revenue integrity. A holistic revenue integrity program enhances the accuracy of charge capture by ensuring that clinical documentation aligns with billed services. Ultimately, optimized revenue capture leads to improved cash flow, better financial performance, and increased resources for patient care and operational investments.
Risk Mitigation
One of the most critical aspects of revenue integrity is mitigating risks that can result in financial penalties, lost revenue, or reputational damage. In an era of heightened regulatory scrutiny, a comprehensive risk management approach within the revenue integrity framework can help identify, address, and mitigate these risks before they escalate. Continuous risk monitoring and real-time analytics allow organizations to detect potential compliance issues early, preventing costly errors before they occur.
Workforce Productivity
Workforce productivity is a key driver of both operational efficiency and financial performance in healthcare organizations. A holistic revenue integrity system empowers healthcare professionals by streamlining processes, reducing manual tasks, and enabling data-driven decision-making. By automating routine processes such as coding, charge capture, and compliance checks, organizations can free up valuable time for their teams to focus on higher-value tasks.
Revenue integrity systems equipped with advanced tools like machine learning and AI can assist coding professionals and compliance officers by flagging potential errors or areas of concern before they become larger issues. This reduces the time spent on reworking or correcting denied claims and increases the accuracy and speed of the revenue cycle.
Additionally, when healthcare professionals have access to accurate, integrated data from a single source of truth, they are better equipped to collaborate across departments, resolve issues efficiently, and contribute to the overall financial health of the organization. Enhancing workforce productivity in this way reduces burnout and turnover while boosting morale and job satisfaction.
Payer Management
Effective payer management is essential for optimizing revenue cycles and ensuring timely, accurate reimbursements. Healthcare organizations must navigate complex payer rules, contract terms, and claim submission requirements to minimize denials and delays in payment. A holistic revenue integrity system helps organizations improve their relationships with payers.
With data-driven insights into payer performance, organizations can monitor trends in claim approvals and denials, identify root causes of recurring issues, and develop strategies to reduce denial rates. This enables more efficient negotiation and communication with payers, leading to faster reimbursement cycles and improved cash flow.
About MDaudit
MDaudit’s continuous risk monitoring technology and platform plays a pivotal role in enhancing revenue integrity for healthcare organizations. Our solutions are designed to support healthcare billing compliance, revenue integrity, and Health Information Management (HIM)/coding professionals in several ways:
Automated Audits: Our platform automates the auditing process, identifying potential risks and discrepancies in real-time, which helps in proactively addressing issues before they escalate.
Comprehensive Reporting: Detailed reports provide insights into billing practices, helping organizations pinpoint areas for improvement and ensuring compliance with regulatory standards.
Continuous Risk Monitoring: By providing continuous risk monitoring capabilities across the healthcare revenue cycle management continuum, billing, coding, and revenue risks can be revealed and mediated.
Educational Resources: We offer training and resources to keep healthcare professionals updated on the latest coding standards and compliance requirements.
Scalability: Our solutions are scalable, catering to healthcare settings of all sizes, from small clinics to large hospital networks.
At MDaudit, we are committed to supporting healthcare providers in achieving revenue integrity success through our advanced technology and comprehensive solutions.