Claim denials represent a significant challenge that can impede financial performance and operational efficiency. One survey showed the top three reasons for an increase in claim denials were insufficient data analytics (62%), lack of automation in the claims/denial process (61%), and lack of thorough training (46%).
When resources are spread thin for revenue integrity teams, strategic and customized insights are necessary to ensure accurate reimbursement and billing compliance.
6 Claim Denial Reports for Revenue Integrity Teams
Reporting is a valuable tool for uncovering claim denial insights. These six claim denial reports can be generated from a credible denial management platform. By leveraging them revenue integrity teams can proactively manage denials, optimize revenue, and enhance overall financial health.
- Denial Rate by Payor Report: A comprehensive overview of denial rates across different payors is essential. By analyzing denial rates by payor, revenue integrity teams can identify patterns, trends, and discrepancies in reimbursement processes. This insight enables targeted interventions, and process improvements tailored to minimize denial trends from specific payors.
- Top Denial Reasons Analysis: Understanding the root causes of claim denials is essential for implementing effective corrective actions. A top denial reasons analysis will categorize denials based on their primary causes, such as coding errors, eligibility issues, lack of documentation, or improper billing practices. Revenue integrity teams can prioritize areas for improvement based on the most frequent denial reasons, implement training programs, and enhance billing workflows to mitigate future denials.
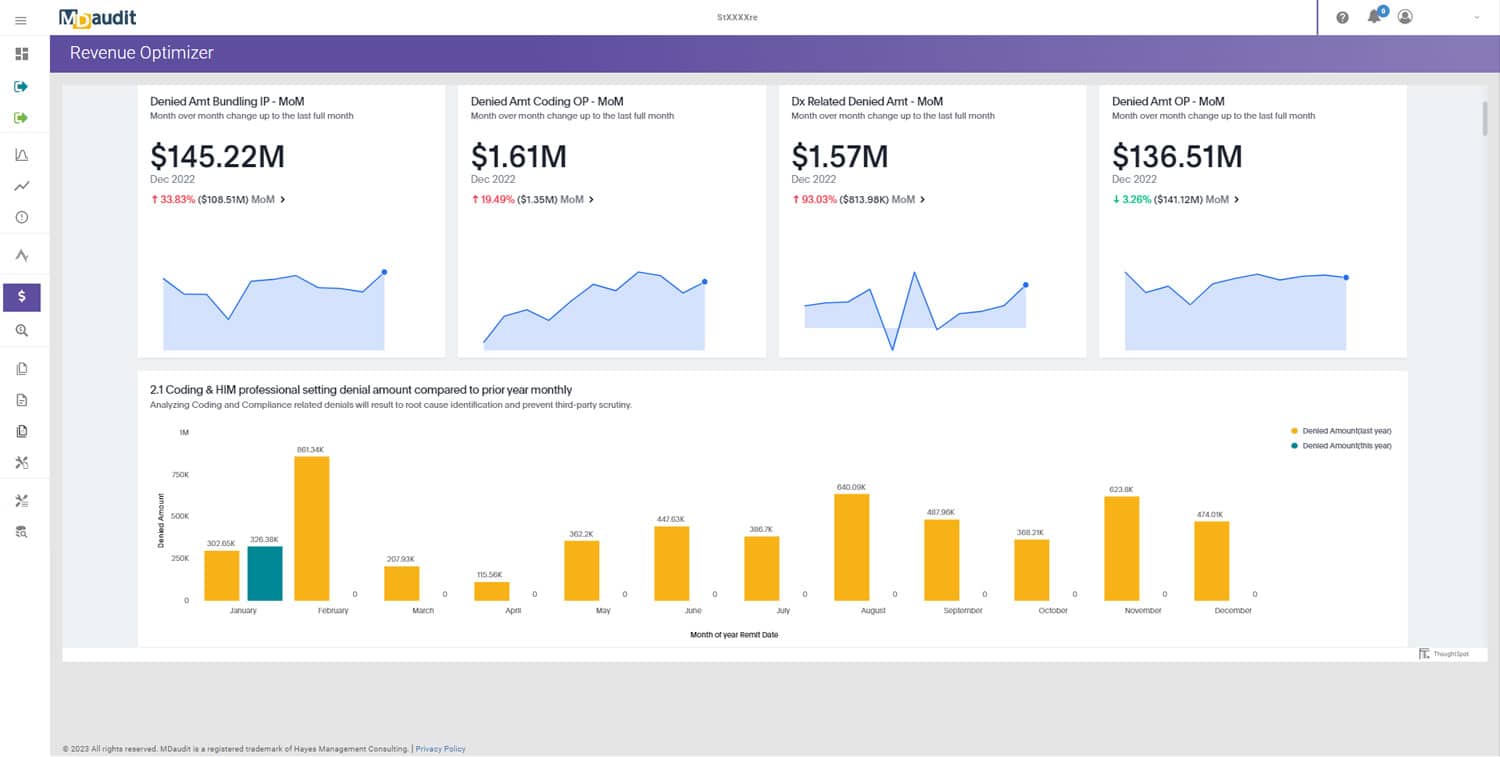
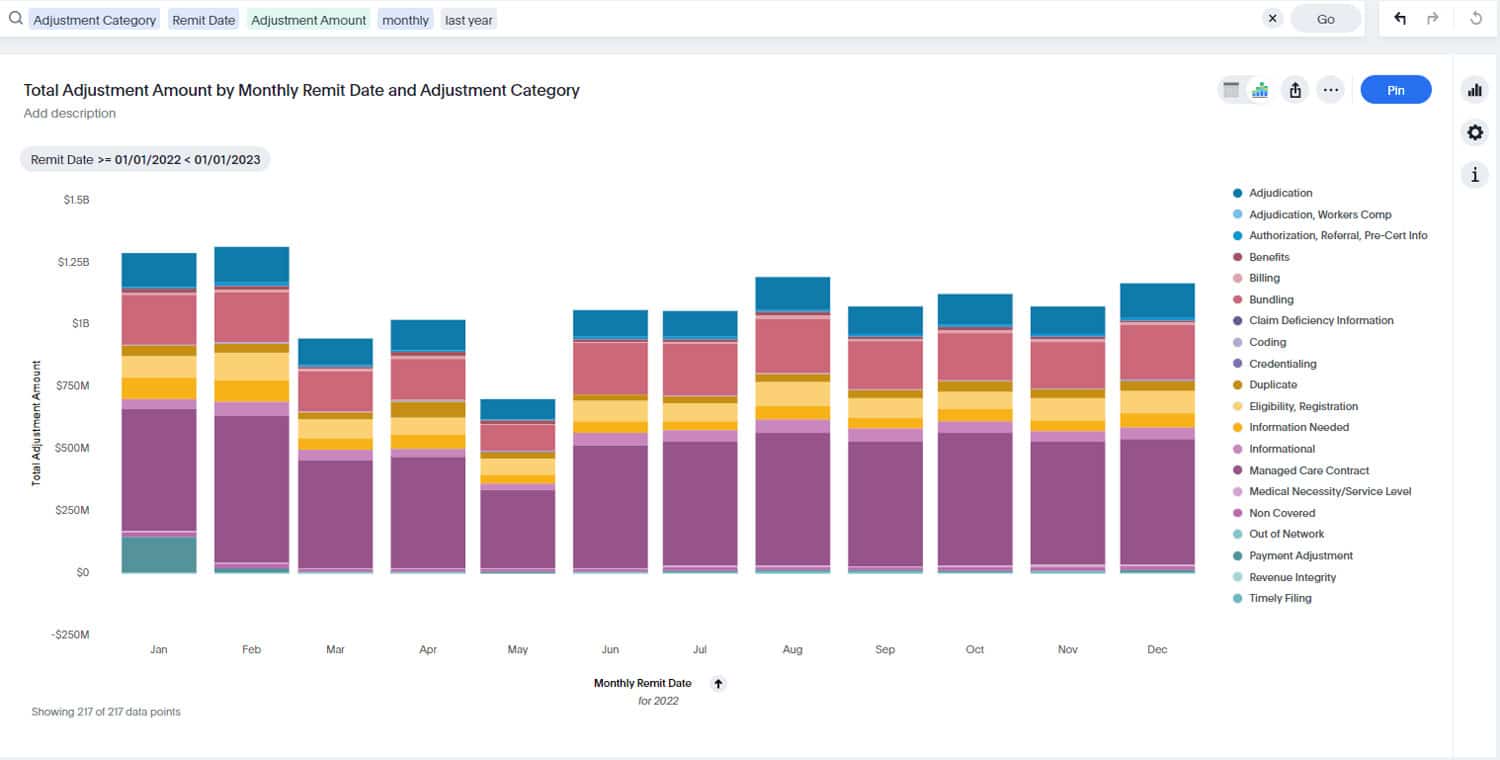
- Trend Analysis of Denial Rates: Analyzing denial rate trends over time is crucial for assessing the effectiveness of denial management strategies. Trend analysis reports visualize denial rate fluctuations, seasonal patterns, and year-over-year comparisons. Revenue Integrity teams can leverage this data to identify improvement opportunities, monitor the impact of intervention initiatives, and adjust denial prevention strategies accordingly.
- Provider-Specific Denial Metrics: Different providers within a healthcare organization may experience varying denial rates and patterns. Provider-specific denial metrics reports segment denials by individual providers, departments, or specialties. This granular insight enables targeted provider education, performance feedback, and process optimizations tailored to address specific denial challenges at the provider level.
- Denial Recovery and Appeals Tracking: Tracking denial recovery and appeals processes is essential for maximizing revenue recapture. Denial recovery reports quantify the amount of denied revenue successfully recovered through appeals or resubmissions. Revenue integrity teams can monitor denial recovery rates, track appeal outcomes, and implement strategies to improve appeal success rates, ultimately minimizing revenue loss due to denials.
- Comparative Analysis with Industry Benchmarks: Benchmarking denial metrics against your peers provides context for performance evaluation. Comparative analysis reports benchmark denial rates, denial reasons, and denial resolution timelines against industry peers or established benchmarks. Revenue Integrity teams can identify areas of competitive advantage, benchmark performance improvement initiatives, and strive for industry-leading denial management practices.
Strategic reporting provides actionable insights to help your revenue integrity teams make informed decisions contributing to a healthier bottom line.