THE CUSTOMER PROFILE
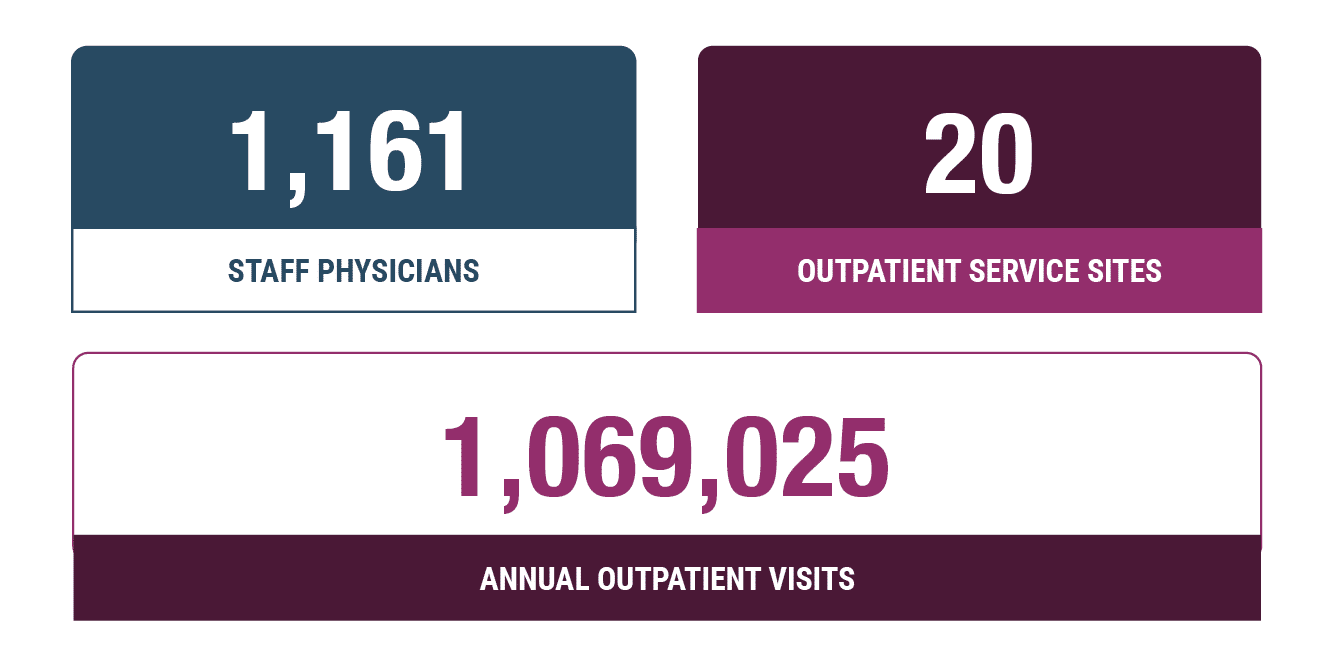
Serving central Indiana since 1859, Eskenazi Health is one of the largest healthcare systems in the U.S., with more than 1 million outpatient visits each year. Eskenazi Medical Group (EMG), a 501(c)(3) aligned with Eskenazi Health, staffs many of the system’s providers. Through a faculty practice plan, EMG partners with the Indiana University School of Medicine, providing flexibility for teaching and research.
EMG features a diverse provider population with “three to four times the national average of Latino providers and two-and-a-half times the national average of African American providers,” according to their website. With a mission to advocate, care, teach, and serve, EMG providers offer care in the 333-bed hospital and across more than 30 area primary and mental health care sites, including numerous federally qualified health centers (FQHCs).
THE CHALLENGE
The newly launched professional revenue integrity program needed a more accurate and efficient way to conduct audits.
Though Eskenazi had a hospital billing (HB) revenue integrity program for over a decade, the professional billing (PB) revenue integrity team was more recently launched to mirror the HB program’s success in improving hospital revenue and charge accuracy. The department’s focus is completing audits and providing feedback for all providers, including E&M documentation, charging accuracy, and improvement initiatives. When issues arise, the team works with the various affected departments to resolve them.
“The main goal is to ensure that we are charging appropriately, that documentation reflects what was actually done, and that we’re capturing everything correctly,” explains Astra Morris, manager of professional revenue integrity. “As a county hospital with several affiliated federally qualified health care centers, we can decrease our reliance on subsidies while continuing to deliver quality care to low-income and at-risk populations by protecting revenue for the institution.”
When the PB revenue integrity department launched, the team used a complex, manual system to conduct audits. “It was very confusing and time consuming,” remembers Morris. Without the ability to analyze charges or identify risk areas, audits were manually randomized in spreadsheets using exported reports from their EHR system. With responsibility for approximately 500 providers, Morris explains, “I estimated it would take three to four years to audit all our providers. I said this just doesn’t work. We have to come up with something.”
With our old system, I estimated it would take three to four years to audit all our providers. I said this just doesn’t work. We have to come up with something.
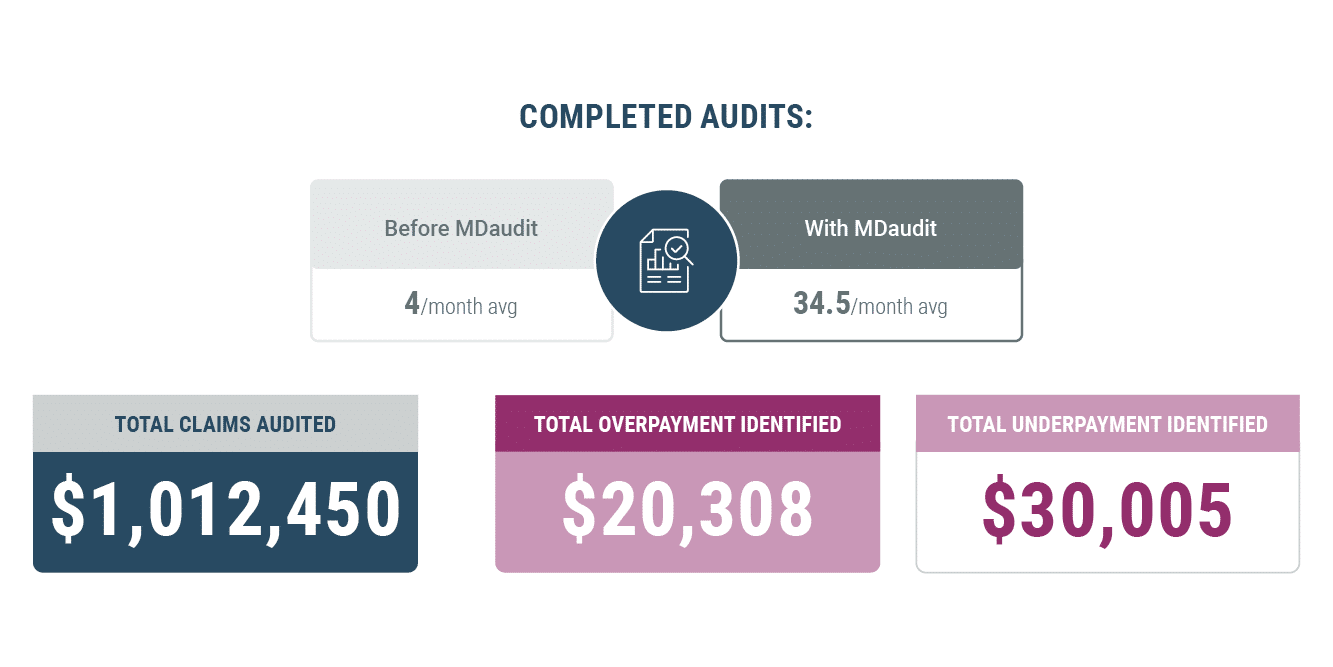
We were only able to do an average of four audits per month per team member with the old system, and now it’s nearly 40 in a month. MDaudit makes the auditing process a whole lot simpler, a lot more streamlined, and much, much faster with higher quality.
THE SOLUTION
MDaudit exponentially increased the number of audits completed.
With MDaudit, Eskenazi has audited more providers, more claims, and more total charges – with more than $1 million reviewed in the past year. “We were only able to do an average of four audits per month per team member with the old system, and now it’s nearly 40 in a month,” says Morris. “MDaudit makes the auditing process a whole lot simpler, a lot more streamlined, and much, much faster with higher quality.”
Morris describes the benefits of MDaudit across the health system: “Obviously, my team has benefited from MDaudit quite a bit because it’s much less stressful on us than it was before.” She explains that providers have also responded favorably to the easy-to-read audit reports and follow-up education.
In addition to standard and ad hoc reporting, Eskenazi leadership can easily identify provider acknowledgments of audit findings, education delivered to providers as a result of an audit finding or other issue, and related turnaround times using MDaudit’s task tracking and reporting to manage deadlines and coordinate activities.
Like many health systems, Eskenazi’s revenue integrity programs are increasingly partnering with other internal departments – including compliance, coding, and revenue optimization – breaking down silos across the organization. MDaudit serves as a centralizing tool, offering data and insights crucial to the various departments.
With all providers audited and increased bandwidth now available to focus on higher-impact matters, the team is able to turn its attention to denials and risk analytics, and other expanded system functionalities. Using audit insights based on actual findings, MDaudit offers the ability to identify and resolve problem areas in one platform.
Morris describes the health systems partnership with MDaudit and the company’s responsiveness to product enhancement requests. “One thing that comes to mind that we requested was increased support for dental for some of our FQHCs and now that is supported.” MDaudit listened to their needs, adding dental codes into the system; more advanced dental features are being developed.
And when Indiana Medicaid’s changing billing and claim presentation rules caused some confusion for Eskenazi, “The team at MDaudit worked through that with us and I’ve been very appreciative of that.”
“I don’t know how I ever got along without MDaudit,” says Morris.
THE RESULTS
Prior to MDaudit, reporting was done with multiple spreadsheets that were difficult to use, messy, and time consuming. With MDaudit, reporting is done with Audit Packages for providers, curated Audit Reports, and Management Reports for leadership.
To download the full case study PDF, click here.