When I wrote this blog at the end of 2019 laying out our MDaudit Enterprise platform vision, I never had imagined a 2020 with a global pandemic. The technology leadership team at Hayes had spent the last quarter of 2019 developing and socializing an extensive platform roadmap with our cross functional partners that would drive significant growth for Hayes and value for our customers.
When COVID-19 hit in the early months of 2020, many changes came at us fast. Like other enterprises, we pivoted to a new mode of working remotely. This brought many new challenges with collaboration, communication and engagement within and outside our organization. Simple things we used to take for granted before the pandemic became pain points – not using the whiteboard, checking in on a colleague, walking into someone’s office to brainstorm a complex problem, celebrating successes and learning from failures, all in-person. Our teams quickly pivoted in a very agile manner to meet the business demands in the new environment.
As we served many large healthcare organizations with our platform in helping them mitigate billing compliance and revenue risks, we found ourselves in a unique situation where we could make a profound impact in helping our customers manage their operations effectively during the pandemic if (a big “IF”) we could successfully pivot from the initially planned 2020 roadmap with a bold incremental agenda that would solve for the macro level trends and signals in the industry. Incrementalism is often panned in the innovation arena but it’s often the path to value-based outcomes in the healthcare industry.
Below are 5 things which did not plan initially for MDaudit Enterprise in the year 2020 but pivoted to innovate under crisis and drive value for our customers.
1. COVID-19 Specific Functionality
When the pandemic hit there was widespread confusion around COVID-19 diagnosis, treatments and billing. It took some time before billing and coding guidelines were released from CMS and WHO. We quickly created segmentation models for COVID-19 specific services so that our customers have the ability to search for those specific services, investigate and fix them to comply with all the regulations and get paid in a timely manner. All through the year, as these guidelines changed, a dedicated team within Hayes kept the segmentation models updated. At the end of 2020, approximately ~$1B worth of gross charges for COVID-19 related services have been audited with our platform covering 10K+ providers and 1.3K+ facilities. Never did we imagine that a functionality that was born out a crisis and rapid brainstorming sessions would drive so much value.
2. Solving for Coding Issues
One of the first signals we picked up from our data in Q1 2020 told us there is financial trouble brewing for healthcare organizations in getting paid in a timely manner during the pandemic. We observed that the denials due to coding issues in Q1 of 2020 was 25% more than in the Q1 2019. We embarked upon an initiative to develop a productivity workflow that would bring together stakeholders from compliance and coding departments to collaborate and engage in a dialogue to solve for coding issues that can impact timely reimbursements for their organizations. As more of our customers were starting to work remotely as well, we also introduced tools that would help them collaborate with their colleagues and peer review their work. The fact that our platform was deployed on the cloud gave them opportunities to deploy their resources on a flexible work schedule including weekends. At the end of 2020, there were more than 2K+ coders and compliance professionals in our system driving collaboration.
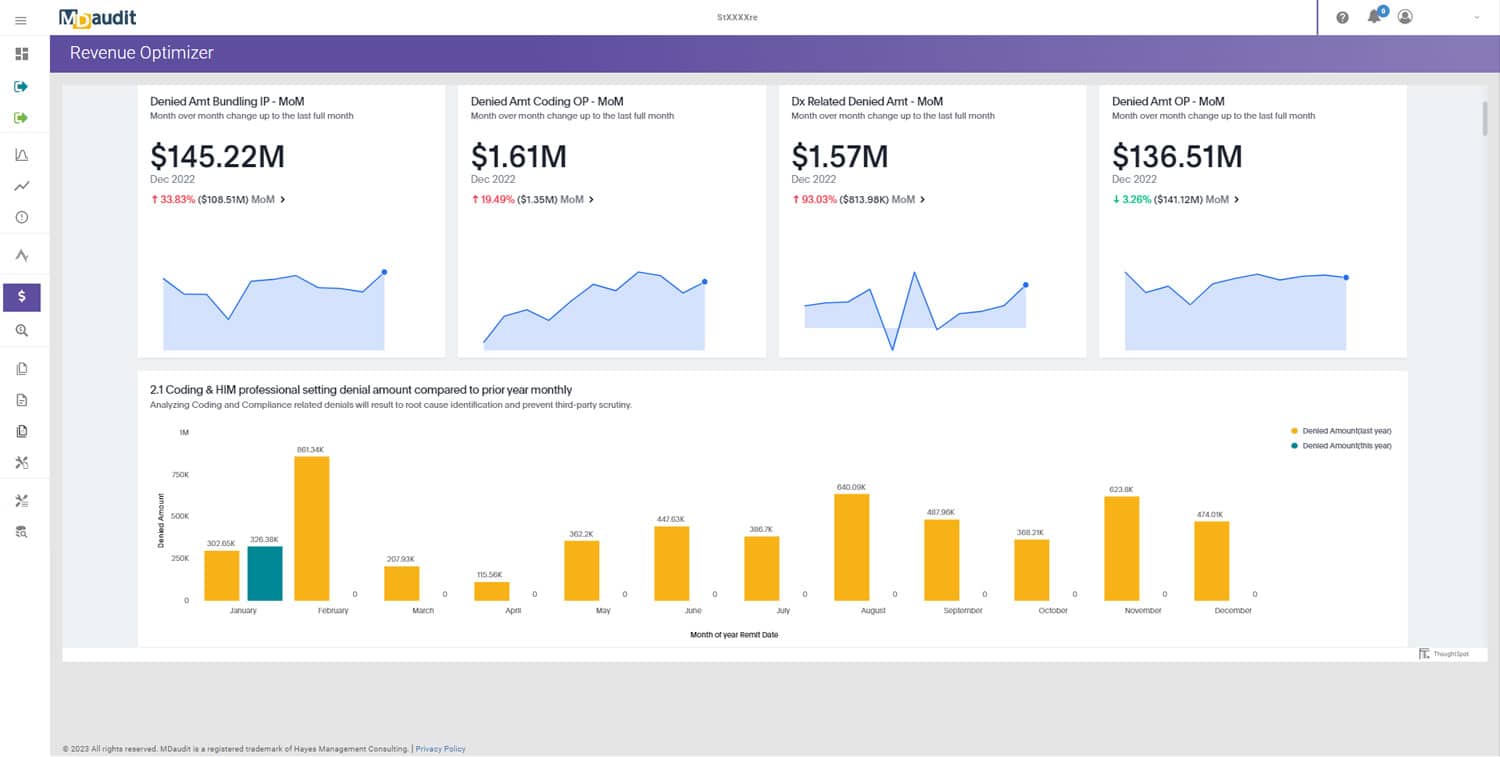
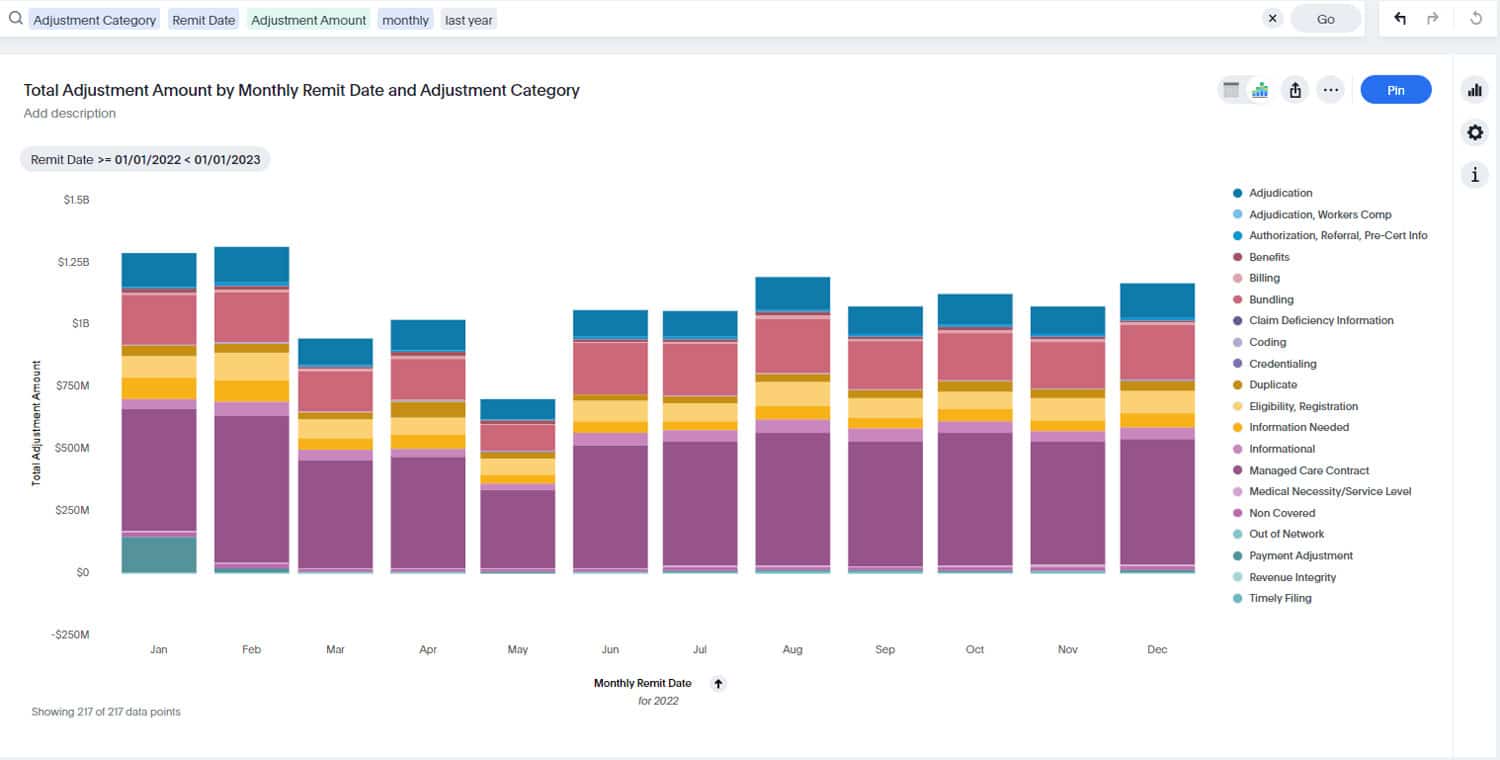
3. Leveraging Augmented Intelligence (AI) to Solve for Revenue Challenges
Most of the AI applications suffer inertia and ultimately fail because technology leads and the problem statements take a back seat. For us at Hayes, we were always focused on our quest towards good problem statements to begin our AI journey in 2020. What’s better than a crisis in finding good problem statements? We hacked our way into many ideas and zeroed in on the issue of Denials in the industry (to quantify, it’s a $250B+ problem in the industry). Our hypothesis was since the elective surgeries were down by double digit percentages and with increasing supply chain costs during COVID-19, healthcare organizations need to get paid in a timely manner for the services they offered to remain financially viable. We finally landed on a solution called ‘Revenue Optimizer’, activated work streams and took this concept to market in mere 12 weeks. Our customers can leverage Revenue Optimizer to analyze millions of rows of data in real time to understand drivers for their denial volumes and dollars and rapidly address the issues to get reimbursed in a timely manner. We also had to solve for the ‘cold start’ problem since many of historical assumptions for our forecasting models had to be optimized to fit the 2020 context. At the end of 2020, approximately $45B of denials have gone through Revenue Optimizer.
4. Proactively Addressing Complex Hospital Inpatient Charges
Hospital claims with inpatient stays are normally complex due to the nature of underlying patient conditions, related services and charges. Last year, the pandemic exacerbated this segment of claims since we had increasing hospitalization and inpatient stays due to COVID-19. We saw that in our MDaudit cohort of customers, hospital services which had CC/MCC and HCC coding were contributing to approximately $6B worth of denials. DRG codes 871 and 870 alone drove 10% of that total number. We introduced segmentation logic in the platform so that our customers can rapidly isolate and identify these hospital inpatient complex claims and investigate them for accuracies in coding and charges proactively or retrospectively to get reimbursed by Medicare or commercial payers in a timely manner. Many of these charges will continue to attract RAC and external audits in 2021 and beyond from federal, state and commercial payers due to its reimbursement dollars at stake.
5. Collaborating With Our Strategic Partners
At Hayes, when we confront problem statements, we don’t pretend to know it all. Last year, we initiated strategic relationships in targeted technology and business areas to learn from our innovation partners in the ecosystem and boost our capabilities such as augmented intelligence, denials prediction and security credentials. Denials prediction is a problem area where we see lots of potential in our initial innovation pilots. Last year alone, we saw that around ~$9B worth of claims were denied for generic reasons in our customer cohort. Many of our customers are trying to solve how they can proactively resolve issues related to clinical and financial information in their claims before they reach the payer so they can accelerate their cash flow in a post pandemic recovery. We will continue to evolve in these areas this year to drive more value to our customers.
In summary, none of the above pursuits would have possible without the dedicated effort of all the team members at Hayes who overcame immense personal and professional challenges to execute with relentless focus and deliver value to our customers during the pandemic. Across all our internal functions at Hayes from R&D to Customer Facing to Corporate, when it comes to innovation, the old adage of “the whole is greater than sum of its parts” holds very true. We fail fast, learn and use incremental insights as steppingstone to the successful outcome.